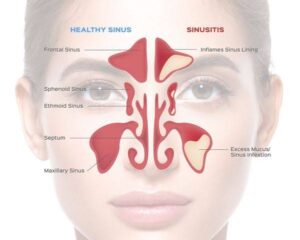
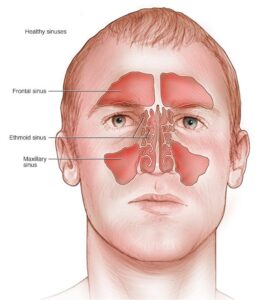
MAXILLARY SINUSITIS

Maxillary sinusitis, an acute or chronic inflammation of the maxillary sinus, is often due to direct extension of dental infection, but originates also from infectious diseases due to bacteria, fungus, or virus such as the common cold, influenza and the exanthematous diseases; from local spread of infection in the adjoining frontal or paranasal sinuses; or from traumatic injury of the sinuses with a superimposed infection. The common organisms include Streptococcal pneumoniae, Hemophilus influenzae, Moraxella catarrhalis in children, gram-negative bacilli, anerobic organisms, rhinovirus and parainfluenza viruses, etc. The occurrence of maxillary sinusitis as a result of the exten- sion of dental infection is dependent, to a great extent, upon the relation and proximity of the second premolar, the first and second molar teeth to the sinus. When sinusitis is secondary to dental infection, the microorganisms associated with the sinusitis are the same as those associated with the dental infection. Apart from periapical infection, foreign bodies, tumors, and granulomatous lesions of the nasomaxillary complex may also produce maxillary sinusitis.
ACUTE MAXILLARY SINUSITIS
Acute sinusitis may result from an acute periapical abscess or acute exacerbation of a chronic inflam- matory periapical lesion, which involves the sinus through direct extension. In some cases a latent chronic sinusitis may be awakened by extraction of a maxillary bicuspid or molar and perforation of the sinus. Usually, the organisms involved in acute sinusitis are S. pneumoniae, H. influenzae, and Moraxella catarrhalis.
Clinical Features
Patients with acute maxillary sinusitis suffer from moderate to severe pain with swelling overlying the sinus. Pressing over the maxilla increases the pain. Often, the painful sensation is one of pressure. Pain may be referred to various areas, including the cheek, posterior teeth and ear. Sinus pain increases when the patient bends over or is supine. The patient may complain of a discharge of pus into the nose and often a fetid breath. Fever and malaise are usually present. The diagnosis of acute maxillary sinusitis from clinical manifestations alone is quite difficult.
Diagnosis
Clinical signs and symptoms, transillumination with strong flashlight in dark room, sinus view radiograph, and computed tomography are some aids that can be used in diagnosis.
Histologic Features
The lining of the maxillary sinus may show a typical acute inflammatory infiltrate with edema of the connective tissue and often hemorrhage. A squamous metaplasia of the specialized ciliated columnar epithelium occurs sometimes.
Treatment and Prognosis
The prime objective of treatment is the removal of the infecting locus. This is particularly efficacious if the infection is of dental origin. Because of the infection present, antibiotics should also be administered. Healing is usually uneventful when this is done.
CHRONIC MAXILLARY SINUSITIS
Chronic sinusitis may develop as the acute lesion subsides or may represent a chronic lesion from the onset.
Common predisposing factors are recent upper respiratory viral infections or allergic sinusitis. In cases of acute or chronic maxillary sinusitis, the possibility of phycomycosis infection (q.v.) must always be considered, especially in diabetic patients. In chronic sinusitis, the organisms are anaerobes and streptococcus, bacteroides, or veil- lonella are the most commonly involved.
Clinical Features
Clinical symptoms of chronic sinusitis may be generally lacking, and the condition may be discovered only during routine examination. Sometimes headache, fever, vague facial pain or upper toothache is present, or there is a stuffy sensation on the affected side of the face. There may be a mild discharge of pus into the nose and a fetid breath. Children may have persistent cough, fever, and purulent rhinorrhea. In chronic sinusitis, rarely will there be dystrophic calcifica- tion termed antrolith, which may be detected radi- ographically.
Roentgenographic Features
Sinusitis can be seen on the roentgenogram as a clouding of the sinus due to the hyperplastic tissue or fluid pres- ent. Films of both sinuses should be compared before a diagnosis is attempted.
Histologic Features
The mucosa lining the maxillary sinus may show remarkable thickening and the development of numerous sinus ‘polyps These polyps are simply hyperplastic granulation tissue with lymphocytic and sometimes plasma cell infiltration. This tissue, which is usually covered by ciliated columnar epithelium, tends to fill the sinus and obliterate it. In some instances there is no remarkable proliferation of granulation tissue; rather, there is only a mild lymphocytic infiltration of the lining tissue with squamous metaplasia of the epithelium.
Treatment and Prognosis
The treatment for chronic maxillary sinusitis consists in removal of the cause of the disease. The prognosis is considered good if the disease is due to dental infection, since it can be eliminated. Infection from other sites may be difficult to eradicate.