
Basa cell adenocarcinoma of salivary glands is an uncommon and recently described entity occurring almost exclusively at the major salivary glands. It is a low grade malignant neoplasm that is cytologically similar to basal cell adenoma, but is infiltrative and has a small potential for metastasis.
Clinical Features.
In AFIP case files spanning almost 11 years, basal cell carcinoma comprised 1.6 per cent of all salivary gland neoplasms and 2.9 per cent of salivary gland malignancies. Nearly 90 per cent of tumors occurred in the parotid gland. The average age of patients is reported to be 60 years. Basal cell adenocarcinoma predominantly occurs at the seventh decade without gender preference. The tumors affecting the minor salivary glands occur most frequently at the oral cavity (buccal mucosa, palate) and the upper respiratory tract. Similar to most salivary gland neoplasms, swelling is typically the only sign or symptom experienced. A sudden increase in size may occur in a few patients.
Histologic Features.
As seen with basal cell adenoma, basal cell adenocarcinoma can also be histologically divided into four subtypes: (a) solid,
(b) ductal,
(c) trabecular, and
(d) membranous.
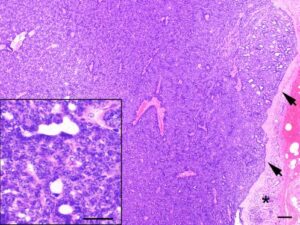
The prevalent histologic tumor pattern is represented by solid neoplastic aggregates with a peripheral cell palisading arrangement frequently delineated by basement membranelike material. Few areas with trabecular or membranous arrangement may be seen. The neoplastic clusters are formed by two cell populations: the small dark cell type, which is predominant and a large pale cell type. Generally, the small dark cells are present peripherally to the larger paler cells. The tumor extends into the surrounding tissues by local infiltration as nodules, nests and cords. Perineural and vascular invasion is noticed in a few cases.
Treatment and Prognosis.
Basal cell carcinomas are low-grade carcinomas that are infiltrative, locally destructive, and tend to recur. They only occasionally metastasize. Surgical excision with a wide enough margin to ensure complete removal of the tumor is the primary treatment. Regional lymph node dissection is recommended only if there is evidence of metastatic disease. The overall prognosis for patients with this tumor is good.
SEBACEOUS CARCINOMA
It is a malignant neoplasm consisting chiefly of sebaceous cells, which are arranged in sheets and/or nests with different degrees of pleomorphism, nuclear atypia and invasiveness.
Clinical Features.
This tumor shows bimodal age distribution, peak incidence of tumor occurrence is found in the third decade and seventh and eighth decades of life (range 17-93 years). The male and female incidence of occurrence is almost equal. Most of the reported cases have arisen in the parotid gland. The chief complaint is that of painful masses, with varying degrees of facial nerve paralysis, and occasionally, fixation of the skin is present. Tumors range in size from 0.6-8.5 cm in greatest dimension.
Histologic Features.
Tumors are well circumscribed or partially encapsulated, with pushing or locally infiltrating margins. Cellular pleomor- phism and cellular atypia are uniformly present and are more prevalent than in sebaceous adenomas. Tumor cells may be arranged in multiple large foci or in sheets and have hyperchromatic nuclei surrounded by abundant clear to cosinophilic cytoplasm. Areas of cellular necrosis and fibrosis are commonly found. Perineural invasion has been observed in more than 20 per cent of tumors. Vascular invasion is extremely unusual. Rare oncocytes and foreign body giant cells with histiocytes may be observed.
Treatment.
It varies from local excision and parotidectomy to preoperative and postoperative radiotherapy, with or without chemotherapy. Patient survival ranged from 8 months to 13 years (mean is 4.5 years).