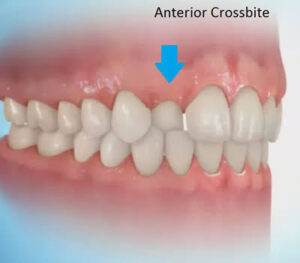
Anterior crossbite, particularly crossbite of all of the incisors, is rarely found in children who do not have a skeletal Class III jaw relationship. A crossbite relationship of one or two anterior teeth, however, may develop in a child who has good facial proportions. When racial/ethnic groups in the U.S. population are combined, about 3% of children have an anterior crossbite in the mixed dentition .
In planning treatment for anterior crossbites, it is critically important to differentiate skeletal problems of deficient maxillary or excessive mandibular growth from crossbites. due only to displacement of teeth.” If the problem is truly skeletal, simply changing the incisor position is inadequate treatment, especially in more severe cases .
Anterior crossbite affecting only one or two teeth almost always is due to lingually displaced maxillary central or lateral incisors. These teeth tend to erupt to the lingual because of the lingual position of the developing tooth buds and may be trapped in that location, especially if there is not enough space. Sometimes, central incisors are involved because they were deflected toward a lingual erup- tion path by supernumerary anterior teeth or overretained primary incisors. More rarely, trauma to maxillary primary teeth reorients a permanent tooth bud or buds lingually.
The most common etiologic factor for nonskeletal anterior crossbites is lack of space for the permanent incisors, and it is important to focus the treatment plan on manage- ment of the total space situation, not just the crossbite. If the developing crossbite is discovered before eruption is com- plete and overbite has not been established, the adjacent primary teeth can be extracted to provide the necessary space .
Treatment of Nonskeletal Anterior Crossbite :-

Lingually positioned incisors limit lateral jaw movements, and they or their mandibular counterparts sometimes suffer significant incisal abrasion. In addition, when oral hygiene is less than ideal and gingival inflammation occurs,
anterior teeth that are in crossbite, especially the lower incisors, are likely to have gingival recession. So, for these reasons, early correction of this type of anterior crossbite is indicated.
Only occasionally is it indicated to correct anterior crossbite in the primary dentition by moving the primary teeth because crowding severe enough to cause it is rare and the teeth often exfoliate before they can be successfully moved. Dental anterior crossbites typically develop as the perma- nent incisors erupt. Those diagnosed after overbite is established require appliance therapy for correction. The first concern is adequate space for tooth movement, which usually requires reducing the width of some teeth, extraction of the adjacent primary teeth, or opening space orthodontically. The diagnostic evaluation should determine whether tipping will provide appropriate correction. Often it will because the problem arose as eruption paths were deflected. If teeth are tipped when bodily movement is required, stability of the result is questionable.
In a young child, one way to tip the maxillary and man- dibular anterior teeth out of crossbite is with a removable appliance, using fingersprings for facial movement of maxillary incisors or, less frequently, an active labial bow for lingual movement of mandibular incisors. Two maxillary anterior teeth can be moved facially with one 22-mil double-helical cantilever spring. The appliance should have multiple clasps for retention, but a labial bow is usually contraindicated because it can interfere with facial move- ment of the incisors and would add little or no retention.
An anterior or posterior biteplate, or bonded adhesive on the occlusal surfaces of posterior teeth to reduce the overbite while the crossbite is being corrected, usually is not necessary in children. Unless the overbite is exceptionally deep, a biteplate would be needed only in a child with a clenching or grinding habit. A reasonable approach is to place the removable appliance without a biteplate and attempt tooth movement. If, after 2 months, the teeth in the opposing arch are moving in the same direction as the teeth to which the force is being applied, the bite can be opened by adding orthodontic banding cement to the occlusal surfaces of the lower posterior molars. When the crossbite is corrected, the cement can be removed relatively easily, and it does not require alteration of the appliance. Using a biteplate or opening the bite risks the chance that teeth not in contact with the appliance or the opposing arch will erupt excessively.
A removable appliance of this type requires nearly fulltime wear to be effective and efficient. If the lingual finger- springs are activated 1.5 to 2 mm, they will produce approximately 1 mm of tooth movement in a month. The offending teeth should be slightly overcorrected and retained until overbite is adequate to retain the corrected tooth posi tions. One or 2 months of retention with a passive appliance is usually sufficient. The most common problems associated with these simple removable appliances are lack of patient cooperation, poor design leading to lack of retention, and improper activation.
One of the simplest fixed appliances for correction of maxillary incisors with a moderate anterior crossbite is a maxillary lingual arch with fingersprings. This appliance is indicated for a child with whom compliance problems are anticipated. The springs usually are soldered on the opposite side of the arch from the tooth to be corrected, in order to increase their length. They are most effective if they are approximately 15 mm long. When these springs are acti- vated properly at each monthly visit (advancing the spring about 3 mm), they produce tooth movement at the optimum rate of 1 mm per month. The greatest problems are distor- tion and breakage from poor patient cooperation and poor oral hygiene, which can lead to decalcification and decay.
It also is possible to tip the maxillary incisors forward with a 2 x 4 fixed appliance (2 molar bands, 4 bonded incisor brackets). In the rare instance when there is no skeletal component to the anterior crossbite, this is the best choice for a mixed dentition patient with crowding, rotations, the need for bodily movement, and more permanent teeth in crossbite. When the anterior teeth are bonded and moved prior to permanent canine eruption, it is best to place the lateral incisor brackets with some increased mesial root tip so that the roots of the lateral incisors are not repositioned into the canine path of eruption, with resultant resorption of the lateral incisor roots. If torque or bodily repositioning is needed for these teeth, finishing with a rectangular wire is required even in early mixed dentition treatment. Otherwise, the teeth will tip back into crossbite again.