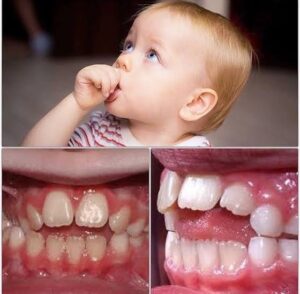
Anterior Open Bite

Oral Habits and Open Bites:-
An open bite in a preadolescent child with normal vertical facial proportions has several possible causes: the normal transition when primary teeth are replaced by the permanent teeth, a habit like finger sucking or tooth displacement by resting soft tissue, or a skeletal problem (excessive vertical growth and rotation of the jaws that would create a disproportionately large lower anterior face height. All told, these problems affect less than 4% of the mixed dentition population. Many of the transitional and habit problems resolve with either time or cessation of the sucking habit. Open bites that persist until adolescence, with the exception of those related to habits, or those that involve more than just the incisors almost always have a significant skeletal component, and careful diagnosis of the contri- buting factors is required. These are termed complex open bites and require advanced treatment methods.
Effects of Sucking Habits :-
During the primary dentition and early mixed dentition years, many children engage in digit and pacifier sucking, with girls predominating. Although it is possible to deform the alveolus and dentition during the primary dentition years with a prolonged and intense habit, much of the effect is on eruption of the permanent anterior teeth. The effect of such a habit on the hard and soft tissues depends on its frequency (hours per day) and duration (months/years). With frequent and prolonged sucking, maxillary incisors are tipped facially, mandibular incisors are tipped lingually, and eruption of some incisors is impeded. As one would expect, overjet increases and overbite decreases. In many children, maxillary intercanine and intermolar width is narrowed, resulting in a posterior crossbite.
When the effect of digit sucking is compared to pacifier use, there is some evidence for increased prevalence of pos- terior crossbites with pacifiers, and especially with pacifier use for more than 18 months. Pacifier shapes that are designed to produce a more physiologic sucking pattern have not been proven to be beneficial when compared with other pacifiers or to finger sucking.” It is also apparent that longer breastfeeding leads to fewer non-nutritive sucking habits.” Most children have a non-nutritive sucking habit at 24 months, but only 40% have one at 36 months. These habits decrease with age and pacifier habits are observed less often with older children than digit habits. The social pressures of school are a strong deterrent.
As long as the habit stops before the eruption of the permanent incisors, most of the changes resolve spontaneously with the exception of posterior crossbite.” By that time, the majority of children have stopped their sucking habit. Another group still suck but want to stop, and yet another small group do not want to stop and appear to be immune to social pressure. If a child does not want to quit sucking, habit therapy (especially appliance therapy) is not indicated.
Nondental Intervention :-
As the time of eruption of the permanent incisors approaches, the simplest approach to habit therapy is a straightforward discussion between the child and the dentist that expresses concern and includes an explanation by the dentist of the problems caused by a prolonged finger habit. This “adult” approach (and restraint from intervention by the parents) may be enough to terminate the habit during this first part of the transition to the permanent dentition but is most effective with older children.
Another level of intervention is reminder therapy. This is for the child who wants to quit but needs help. Any one of several reminders that are introduced with an explanation to the child can be useful. One of the simplest approaches is to secure an adhesive bandage with waterproof tape on the finger that is sucked . The anterior portion of the quad helix appliance also can be quite useful as a reminder when it is placed in the appropriate position in the palate .
If the reminder approach fails, a reward system can be implemented that provides a small tangible daily reward for not engaging in the habit. In some cases, a large reward must be negotiated for complete cessation of the habit.
If all of these fail and the child really wants to quit, an elastic bandage loosely wrapped around the elbow prevents the arm from flexing and the fingers from being sucked. If this is used, wearing it only at night and 6 to 8 weeks of intervention should be sufficient. The child should understand that this is not punishment.
Appliance Therapy :-
If the previous methods have not succeeded in eliminating the habit, a removable reminder appliance is contraindicated because lack of compliance is part of the problem. The child who wants to stop can be fitted with a cemented reminder appliance that impedes sucking . These appliances can be deformed and removed by children who are not compliant and do not truly wish to stop the habit, so cooperation still is important. If this is understood by the child as a “helping hand” rather than punishment, the treatment will be successful and psy- chologic problems will not result. The preferred method is a maxillary lingual arch with an anterior crib device, making it extremely difficult for the child to place the thumb or other object in the mouth.
In about half of the children for whom such a crib is made, thumb-sucking stops immediately and the anterior open bite usually begins to close relatively rapidly thereafter. In the remaining children, thumb-sucking persists for a few weeks, but the crib device is eventually effective in extinguishing thumb-sucking in 85% to 90% of patients.” It is a good idea to leave the crib in place for 6 months after the habit has apparently been eliminated. Commonly, these cemented reminders, like lingual arch expanders, leave an imprint on the tongue that will resolve some time after the appliance is removed. The appliances also trap food and can lead to mouth odor, so excellent oral hygiene is important.
The open bites associated with sucking in children with normal jaw relationships often resolve after sucking stops and the remaining permanent teeth erupt. An appliance to laterally expand a constricted maxillary arch will be required, and flared and spaced incisors may need retraction, but the open bite should require no other treat- ment in children with good skeletal proportions.