
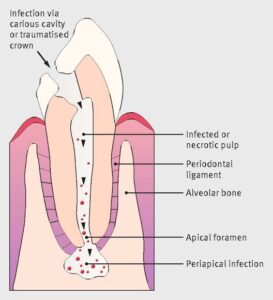
An oral infection may originate in the dental pulp and extend through the root canals and into the periapical tissues, or it may originate in the super- ficial periodontal tissues and subsequently disperse through the spongy bone. Afterwards, it may per- forate the outer cortical bone and spread in various tissue spaces or discharge onto a free mucous membrane or skin surface. It may become local- ized or extend diffusely. The spread of the disease depends upon a variety of factors and circum- stances that may alter its course at any point. Although the intrabony confined infection in itself is serious, it is even more dangerous if the infec- tion escapes from the confines of the bone of the maxilla or the mandible.
The routes by which the infection can spread are: the lymphatic system, the bloodstream or directly through the tissues. Factors affecting the ability of the infection to spread depend on the type and virulence of the organism, general health of the patient, the anatomical site of the initial infection, which decides the drainage of pus, and the effectiveness of the patient’s immune mechanism.
To a large extent, certain anatomic features determine the actual direction that the infection may take .
CELLULITIS (Phlegmon) :
Cellulitis is a diffuse inflammation of soft tissues which is not circumscribed or confined to one area, but which, in contradistinction to the abscess, tends to spread through tissue spaces and along fascial planes. This type of reaction occurs as a result of infection by microorganisms that produces significant amounts of streptokinase, hyaluronidase and fibrinolysins which act to break down or dissolve hyaluronic acid, the universal intercellular cement substance, and fibrin Streptococci are par ticularly potent producers of hyaluronidase and are therefore a common causative organism in cases of cellulitis. The less common hyaluronidase- producing staphylococci are also pathogenic and frequently give rise to cellulitis.
Parh of spread of Infection from acute periapical abscess
Cellulitis of the face and neck most commonly results from dental infection, either as sequela of an apical abscess or osteomyelitis, or following peri odontal infection. The pericoronal infection or peris coronitis (q.v.) occurring around erupting or partially impacted third molars and resulting in cellulitis and trismus is an especially common clinical condition Sometimes cellulitis of the face or neck will occur as a result of infection following a tooth extraction injection, either with an infected needle or through an infected area, or following jaw fracture.
Clinical Features :
The patient with cellulitis of the face or neck originating from a dental infection is usually moderately ill and has elevated tempera- ture and leukocytosis, One feels painful swelling of the soft tissues involved that are firm and brawny. Much of the swelling is due to inflamma tory edema . If the superficial tissue- spaces are involved, the skin is inflamed, has an orange peel appearance and is even purplish some- times. In the case of inflammatory spread of infec tion along deeper planes of cleavage, the overlying skin may be of normal color. In addition, regional lymphadenitis is usually present.

Infections arising in the maxilla perforate the outer cortical layer of bone above the buccinator attachment and cause swelling, initially of the upper half of the face. The diffuse spread, how- ever, soon involves the entire facial area. Extension towards the eye is a potentially serious complica- tion because of the cavernous sinus thrombosis through the veins of the inner canthus of the eye. When infection in the mandible perforates the outer cortical plate below the buccinator attach- ment, there is a diffuse swelling of the lower half of the face, which then sees a superior as well as cervical spread. Spread to the cervical tissue can cause respiratory discomfort.
As the typical facial cellulitis persists, the infection frequently tends to become localized, and a facial abscess may form. When this happens, the suppurative material present seeks to ‘point’ or discharge upon a free surface . If early treatment is instituted, a resolution usually occurs without drainage through a break in the skin.
Histologic Features :
A microscopic section through an area of cellulitis shows only a diffuse exu- dation of polymorphonuclear leukocytes and occa- sional lymphocytes, with considerable serous fluid and fibrin, causing separation of connective tissue or muscle fibers . Cellulitis presents only a nonspecific picture of diffuse acute inflammation.
Treatment and Prognosis :
Cellulitis is treated by the administration of antibiotics including anti-anaerobics and the removal of the cause of the infection. To avoid the further spread of infection or solid- ification of abscess, the patients should be advised not to massage the affected area with any medication. Although this condition is extremely serious, the resolution is usually prompt with adequate treatment, and untoward sequelae are uncommon.
Spread of Infection from Maxillary Teeth :
From the central and lateral incisor the infection spreads to form labial, palatal abscess or vestibular abscess. Sometimes abscesses may form within the lip, which depends upon whether the pus pene- trates above or below the muscle attachment.

Cellulitis of maxillary teeth
Infections of the canine tooth may result in labi- al or vestibular abscess if the site of penetration of pus is below the muscle attachment. They form a canine space abscess if the site of penetration of the pus exists above the levator muscle of the upper lip.
Infected premolars form abscesses mostly on the buccal or palatal side, and in a long rooted tooth form canine space abscess.
Infections from molars form buccal or palatal abscess if the site of penetration is below the buc- cinator muscle attachment, and a buccal space abscess if the site of penetration of pus is above the attachment.
Spread of Infection from Mandibular Teeth :
From the incisor, the infection spreads to form a labial abscess if the pus penetrates above the mus- cle attachment, and forms a submental space abscess if it is below the muscle attachment.

Cellulitis of mandibular teeth
Since all the muscle attachments are well below the root apex in canine teeth, the site of the penetration of the pus is above the muscle attach- ment, and forms only a labial or vestibular abscess.
Premolars may form vestibular abscesses, and lingual perforation may form sublingual abscesses.
If the pus from the first molar penetrates above the bucciantor attachment, it forms a vestibular abscess on the buccal side, and below the muscle attachment results in a buccal space abscess. A sub- lingual abscess may be formed if the pus penetrates through the lingual side.
In second molars there are four possibilities, namely a vestibular or buccal space abscess if the pus penetrates through the buccal side, and sublingual or a submandibular abscess if it penetrates through the lingual side. Infections from the third molars form submandibular or pterygomandibular or submasseteric abscesses.
Secondary sites of spread are the parotid space, temporal, infratemporal, and pharyngeal spaces.