- CHRONIC ALVEOLAR ABSCES

It is a long-standing, low grade infection of the periradicular tissues.
Etiopathogenesis
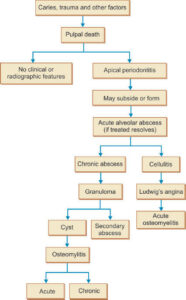
It results from direct extension of acute pulpitis or acute non-suppurative periodontitis or acute exacerbation of periapical granuloma, cyst or chronic abscess.
. The surrounding tissue attempt to localize the pyo- genic infection by forming enclosure of granulation tissue; this in turn is surrounded by fibrous connective tissue; this results in well circumscribed lesion containing necrotic tissue.
Well circumscribed lesion may form sinus due to –
⚫ Inability of the body to completely contain or localized the causative organisms.
Increase in number of causative organisms.
Lowering of patient’s general resistance.
Trauma or surgical intervention.
Enlarging dentoalveolar abscess contains purulent material that is under pressure due to the production of pus. The purulent material travels along path of least resistance, until it reaches the surface, where due to limitation of periosteal layer, it temporally forms subperiosteal abscess. Eventually, it erodes through the periosteum and penetrates the soft tissue, again, following the path of least resistance.
Path of least resistance is determined by the location of breakthrough in the bone and the anatomy of muscles and fascia plane in the area.
Clinical Features
It is characterized by less soreness and often, a better defined radiographic lesion.
History-history of pain that started as dull ache and progressed to severe throbbing type. Sudden decrease in pain signals the formation of sinus.
Signs-tooth is tender, vitality test is negative.
Draining fistulas are also commonly associated with chronic alveolar abscess .
Majority opens on labial and buccal aspect of alveolus, as apices of both maxillary and mandibular teeth are located nearer to the buccal than the lingual cortical plate..
In maxilla, roots of lateral incisors and molars are close to palatal cortical plate, so sinus appear there.
Most root tips lie below the mylohyoid muscle, so pus drains into the submandibular space.
• Lymph nodes-the patients will demonstrate lymphadenopathy as well.
• Location of sinus-sinus opening appears as a small ulcer. It is usually present opposite the root apex in the labial or buccal mucosa; it may be located far away from the affected tooth.
Sinus opening-mucosal sinus opening may be rough and may bleed easily.
Occasionally, after temporary emphysema, sinus heals and form slightly raised pale papule. As the pus accumulates, another signs formation may take place eventually.
Radiographic Features
Lamina dura-there is loss of thickness and density of the apical portion of lamina dura of the affected tooth.
Bone in periapical area-widespread area of diffuse demineralization of the periapical bone, of affected tooth becomes apparent.
Margins-margins vary from well defined with possible hyperostotic borders to poorly defined, in chronic cases. In some areas, margins fade gradually and imperceptibly into the normal bone, while in some there is abrupt demarcation between the normal bone and the radiolucent area.
• Advanced cases after some period, the trabeculae which are rarefied are destroyed and the dark area becomes darker and larger, as more of the surrounding bone is taken into the diseased area.
Adjacent tooth-in some cases, radiolucency may involve adjacent tooth and there may be loss of lamina dura of that tooth.
Side of root-in some cases osteitis can occur at the side of root rather than the apex. The reasons for this are that the infection may spread from adjacent tooth or perforation of the root (while filling the canal) or from an aberrant canal opening.
Maxillary upper posterior teeth-in case of maxillary upper posterior teeth (as they are near to maxillary sinus), the radiographic appearance shows bone destruction at the apex of the tooth, along with loss of lamina dura and with destruction of a portion of the antral floor.
Root-roots of the affected teeth may show resorption.
Histopathological Features
Macrophages and granulation tissue are present.
Lymphocytes and plasma cells are found at the periphery of the abscessed area, with variable number of polymorphonuclear leukocytes at center.
Fibroblast may start to form capsule at the periphery.
Sinus tract is generally lined by granulation tissue. In addition, chronic inflammatory cells are also present.
Differential Diagnosis
Periapical osteofibrosis-it is associated with vital tooth. There may be persistence of lamina dura in the periapical osteofibrosis, even in the presence of well marked bone destruction.
• Foraming-in it, lamina dura is intact. If foramens are exactly superimposed on the roots, then in that cases another radiograph should be taken at different angulation.
Inferior dental canal-it is frequently superimposed on the lower molars and if the canal is dark and apex is small, it is difficult to trace the lamina dura. In this case, magnifying glass should be used to trace the continuity of lamina dura.
A large normal marrow space-it can also be confused if superimposed on the apex of the root. Again, by using magnifying glass lamina dura can be traced.
Management
Antibiotics are seldom used.
If there is need of retention of offending tooth, necrotic pulp should be opened and tooth should be treated endodontically.
The tooth which cannot be restored should be extracted.