
It is also called as pulp polyp or pulpitis aperta. It is essentially an excessive, exuberant proliferation of chronically inflamed dental pulp tissue.
It is a productive pulpal inflammailen due to an extensive carious exposure of a young pulp. It le characterized by the development of granulation tissue, covered at times by epithelium and resufung from long standing low grade infection.
Causes :-
Slow progressive carious exposure of the pulp is the cause.
For the development of a hyperplastic prop, a large open cavity, a young resistant pulp and a chrende low grade stimulus is necessary.
Mechanical irritation from chewing and bacterial infection often provides the stimuli.
Clinical features :-
• Teeth most commonly involved are deciduous molars and first permanent molars as they have an excellent blood supply because of a large root opening and this coupled with high tissue resistance and reactivity in young persons accounts for unusual proliferative properties of the pulp tissue.
It is asymptomatic and it is seen only in teeth of children and young adults.
• Polypoid tissue appears as a fleshy, reddish pulpal mass filling most of the pulp chamber or cavity or even extending beyond the confines of the tooth.
Sometimes, mass if large enough interferes with comfortable closure of teeth.
Polypoid tissue is less sensitive than normal pulp tissue and more sensitive than the gingival tissue.
It may cause discomfort during mastication, due to pressure of food bolus.
This tissue bleeds easily because of rich network of blood vessels.
The tooth may respond feebly or not at all to the thermal test.
There is presence of squamous covering as a result of grafting of exfoliated epithelial cells from adjacent oral mucosa.
Radiographic features :-
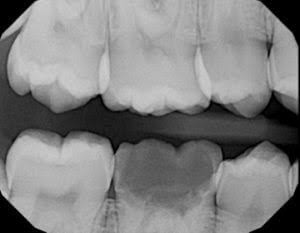
• It will show a large open cavity with direct access to the pulp chamber.
Histopathological features :-
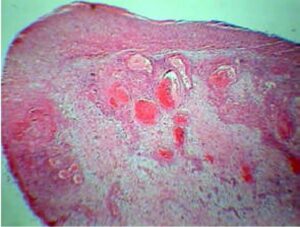
The surface of the pulp polyp is covered by stratified squamous epithelium.
• Such epithelium may be derived from gingiva or freshly desquamate epithelial cells of the oral mucosa or tongue.
The tissue in the pulp chamber is often transformed into granulation tissue which projects from the pulp into the carious lesion.
. The granulation tissue is a young vascular tissue containing polymorphonuclear neutrophils, lymphocytes and plasma cells. The granulation tissue may become epithelized as a result of implantation of epithelial cells on its surface.
Granulation tissue is made up of delicate connective tissue fibers interspersed with a variable number of small capillaries.
Inflammatory cell infiltration chiefly lymphocytes and plasma cells are also seen.
Differential diagnosis :-
Proliferating gingivitis-one should raise and trace the stalk of the tissue back to its origin, i.e. the pulp chamber.
Management :-
• Elimination of polypoid tissue, followed by extirpation of the pulp.
After removing the hyperplastic tissue bleeding can be controlled by pressure.
• Extraction of tooth can also be done.
Pulp Degeneration :-
Degeneration is usually present in older aged people.
Causes :-
It is a result of persistent, mild irritation in teeth of younger people.
Clinical features :-
In early stages, there are no symptoms and no clinical findings.
As degeneration progresses, the tooth may become discolored and the pulp within does not respond to stimuli.
Types :-
Calcific degeneration-a part of pulp tissue is replaced by calcific material that is pulp stones and denticles are formed. The calcific material has a laminated structure like the skin of an onion and lies unattached within the body of pulp. In another type of calcification the calcified material is attached to the wall of the pulp cavity and is an integral part of it.
Atrophic degeneration-it is observed in older people. The pulp tissue is less sensitive than normal.
Fibrous degeneration-it is characterized by replace- ment of the cellular element by fibrous connective tissue. On removal from the root canal, the pulp has the characteristic appearance of a leathery fiber.
Pulp artefacts vacuolization of the odontoblasts was once thought to be a type of pulp degeneration characterized by empty spaces formally occupied by odontoblasts. It is an artefact caused by poor fixation of the tissue specimen..
Tumor metastasis-it is rare except possibly in the terminal stages. It may occur due to direct local extension from the jaw.
Pulp Calcifications :-
Various forms of pulp calcifications are found within the pulp which may be located in the pulp chamber or in the root canals. It can occur in any sex and in any teeth in the dental arch.
Etiology :-
⚫ There is no clear-cut etiology. There is no relation between pulpal inflammation and irritation, as that arising from caries or trauma, since pulp calcification can be found in unerupted teeth.
Extremely high percentage of pulp stones yield pure growth of streptococci on culture but often the affected teeth are normal.
Sundell schematic presentation- local metabolic dysfunction → trauma→ Hyalinization of injured cell → vascular damage → thrombosis vessel wall damage → fibrosis → mineralization (nidus formation) growth-pulp stones.
Classification :-
There are two main forms of pulp calcification:
Discrete pulp stones (denticles, pulp nodules )
It is of following types :-
True denticles-they are made of localized masses of calcified tissue that resembles dentin due to their tubular structure. Tubules are irregular and few in number. More common in pulp chamber than root. canals. They are subdivided into
Free denticle-Denticle lying entirely within pulp tissue and is not attached to the dentinal wall.
Attached denticle-These are continuous with the dentinal wall.
False denticle-it is composed of localized mass of calcified material and they do not exhibit dentinal tubules. Nodule appears to be made up of concentric layers or lamellae deposited around at central nidus. It is composed of cells around which laid down is a layer of reticular fibers that subsequently calcifies. They are again classified as free or attached. They are larger than true denticles and they may fill nearly the entire pulp chamber.
• Interstitial denticle-as the concentric deposition of calcified material continues it approximates and finally is in apposition with the dentinal wall where it may be surrounded by secondary dentin then it is called as an interstitial denticle.
Diffuse calcification :-
It is also called as calcific degeneration.
It is amorphous unorganized linear strands or columns parallel with blood vessels and nerves of pulp.
Clinical significance :-
Sometimes, it may cause pain from mild pulpal neuralgia to severe excruciating pain resembling that of tic douloureux as the denticle can impinge on the nerve of the pulp.
Difficulty may be encountered in extirpating the pulp during root canal therapy.
Radiographic features :-
They are seen as radiopaque structures within the pulp chamber, in the root canals or extending from pulp chamber into root canals.
They may be round or oval.
They may occur as single dense mass or several opacities.
Their outline varies from sharply defined to more diffuse margins
Management :-
Not required.
Reticular atrophy of pulp :-
It is a degenerative or regressive change of pulp.
Etiology :-
• Age changes in elderly person.
Clinical features :-
• Vacuolization of the pulpal tissue and cells.
• A tooth is symptomless and responds normally to vitality test.
Histopathological features :-
• Presence of large vacuolated spaces in the pulp with reduction in the number of cellular element
Degeneration and disappearance of odonlas .
Necrosis of Pulp :-
It is the death of pulp. It may be partial or trial depending on whether a part or the opp involved.
Causes :-
It is sequelae of inflammation and can ao cont following trauma, in which the pulp is desired before an inflammatory reaction.
Types :-
Coagulation necrosis-the soluble portion of tissue is precipitated or is converted into a solid material. Caseation is a form of coagulation necrosis in which the tissue is converted into a cheesy mass consisting chiefly of coagulated proteins, fats, and water.
Liquefaction necrosis-it results when proteolytic enzymes convert the tissue into softened mass, liquid or amorphous debris.
Clinical features :-
• It causes no painful symptoms.
Discoloration of the tooth is the first indication that the pulp is dead.
• The tooth with partial necrosis can respond to thermal changes owing to presence of vital nerve fibers passing through the adjacent inflamed tissue.
History of severe pain lasting from a few minutes to a few hours, followed by complete and sudden cessation of pain.
Histopathological features :-
• Necrotic pulp tissue, cellular debris and micro- organisms may be seen in the pulp cavity.
The periapical tissue may be normal or slight evidence of inflammation of the apical periodontal ligament may be seen.
Management :-
Preparation and obturation of root canals.
Aerodontalgia :-
It occurs due to effect of change in the altitude.
Persons experience pain during high altitude flight or during deep sea diving. At ground level, the tooth is asymptomatic.
It occurs due to subclinical pulpitis.
It may occur in patients with improper obturation as improperly obturated root canal may expand during flight or during diving which creates pressure in the periapical nerve bundles and produce pain.
Cracked Tooth Syndrome :-
Patient complains of pain ranging from mild to excruciating, at the initiation or release of the biting pressure.
It can mimic the condition as severe as trigeminal neuralgia.
A crack may involve enamel and dentine only or it may also involve the pulp and symptoms will vary accordingly.
Pain occurs due to fluid movement within the dentinal tubules causing stimulation of sub- odontoblastic nerve fibers. The fluid movements are induced by pressure changes when biting with the offending cusp.
If the crack involves dental pulp, direct bacterial invasion will occur with predictable pulpal inflammation and resultant pulpitic pain.
Close examination of the crown of the tooth may disclose a crack in enamel, which may be better visualized by using a dye or by transilluminating the tooth with fiber-optic light.
Crack can be confirmed by selective biting pressure using a cotton roll or a small wooden stick to allow selective localization of such pressure.
It is treated by splinting of the offending cusp with a cusp protecting restoration or by removing the split cusp and then restoring the tooth.