
TYPES OF GINGIVITIS
Depending on course and duration.
Depending on distribution.
Depending on the Course and Duration
Acute gingivitis is of sudden onset and short duration and can be painful.
Subacute is a less severe phase of acute condition
Recurrent gingivitis reappears either after treatment or disappears spontaneously.
Chronic gingivitis is slow in onset, of long duration usually painless and the most commonly occurring gingival condition.

Depending on the Distribution
If the condition is involving a single tooth or group of teeth it is called localized gingivitis, while generalized gingivitis involves entire mouth.
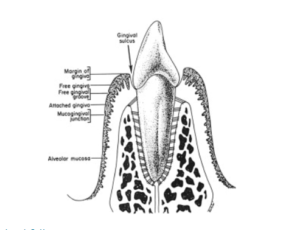
According to distribution, gingivitis could be marginal, papillary or diffuse. If the inflammation is limited to the marginal gingiva, the condition is termed as marginal gingivitis. In papillary gingivitis the inflammation is limited to the interdental papilla. When the inflammation spreads to attached gingiva also, it is termed as diffuse gingivitis, i.e. involving marginal, papilla and attached gingiva. Papillary, marginal and diffuse gingivitis can occur as localized or generalized conditions
CLINICAL FINDINGS
While examining the gingiva clinically, one must adapt a systematic approach. Close attention should be given to any tissue alterations, because they contribute to diagnosis. The gingiva is examined for the following characteristics, color, contour, consistency, size, position, severity of bleeding, surface texture.


Gingival Bleeding on Probing
- Significance of gingival bleeding.
- Etiological factors responsible for gingival bleeding.
- Associated microscopic changes.

Significance of Gingival Bleeding on Probing
- It is one of the earliest visual signs of inflammation
- It can appear earlier than color changes or any other visual signs of inflammation.
- It also provides an additional advantage, by being a more objective sign that requires less subjective estimation by the examiner.
d. Gingival bleeding on probing also helps us to determine whether the lesion is in an active or inactive state. In inactive lesion there will be little or no bleeding on probing, whereas active lesions bleed more readily on probing
e. The severity and ease with which bleeding can be b provoked indicates the intensity of the inflammation.
Etiological Factors Responsible for Gingival Bleeding on Probing
These are divided into:
- Local factors: Those factors that result in acute bleeding.
- Systemic factors: Those factors that cause chronic bleeding.
Acute bleeding is caused due to:
- Tooth brush trauma,
- Impactation of sharp pieces of hard food,
- Gingival burns from hot foods or chemicals, 4. In conditions such as acute necrotizing ulcerative gingivitis (ANUG).
Chronic bleeding: The most common causes are:
- Chronic inflammation due to the presence of plaque and calculus
- Mechanical trauma e.g., from tooth brushing, tooth picks or food impaction.
- Biting into solid foods such as apples.
Systemic factors: include various systemic diseases such as:
- Hemorrhagic diseases including, vitamin C deficiency, vitamin K deficiency, platelet disorders such as thrombocytopenic purpura, other coagulation defects such as hemophilia, leukemia and others.
- Bleeding could also be as a result of excessive administration of drugs such as salicylates and anticoagulants such as dicumarol and heparin.
Microscopic Changes Associated with Gingival Bleeding on Probing
In plaque-induced gingival inflammation, the following histological changes are seen:
a)In the epithelium: Thinning and micro-ulcerations of the sulcular epithelium is seen. Thinning of the epithelium could be due to the toxic substances released by plaque bacteria which destroys the inter- cellular junctions, Micro-ulcerations are as a result of bacteria trying to gain entry into the connective tissue by breaking through the epithelium or in response to inflammation, the neutrophils from the connective tissue cross the epithelial barrier to reach the site of infection, in doing so they cause ulceration in the epithelium or combination of both.
b)In the connective tissue: Dilation and engorgement of the capillaries takes place. Since the capillaries are engorged and closer to the surface which is already thinned and less protective, stimuli that are otherwise innocuous can cause rupture of the capillaries which may result in gingival bleeding.
Color Changes in the Gingiva
Color of the gingiva is an important clinical sign of gingival diseases. Normally gingiva appears to be “coral pink”. The factors that are responsible for this are tissue vascularity,degree of keratinization and thickness of the epithelium. Generally color of the gingiva may change to red, to bluish-red, to pale-pink. When there is increased vascularity or reduced epithelial keratinization, the gingiva becomes more red. The color becomes pale when vascularization is reduced or epithelial keratinization increases. Venous stasis gives a bluish hue to the gingiva.
Changes in the color may start from the interdental papilla and later spread to marginal and attached gingiva. Systemically absorbed heavy metals may also cause gingival pigmentation, e.g. bismuth, arsenic, mercury. lead and silver. Abnormal melanin pigmentation of the gingiva may be observed in conditions like Addison’s disease, Peutz-Jeghers syndrome, Albright’s syndrome and von-Recklinghausen’s disease.
Changes in the Consistency of Gingiva
Normal gingiva exhibits a firm and resilient consistency. Factors that are responsible are cellular and fluid content and collagenous nature of lamina propria. In disease conditions, it can be soggy and edematous or firm and leathery in consistency.
Changes in the Size of the Gingiva
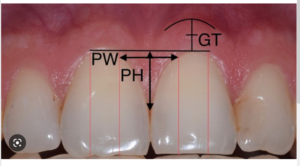
Normal size depends on the sum of the bulk of cellular and intercellular elements and their vascular supply. In disease; the size is increased which can be termed as gingival enlargement. The factors responsible for this are increase in fibers and decrease in cells as in non inflammatory type. Where as in inflammatory type there will be increase in cells and decrease in fibers.
Surface Texture
Under normal conditions, gingiva appears to be stippled (orange peel appearance) due to attachment of gingival fibers to the underlying bone. Microscopically, alternate rounded protuberance and depressions in the gingival layer may give rise to stippled appearance. Stippling is absent in disease conditions, hence the gingiva may appear smooth and shiny.
Changes in the Position of Gingiva
Normally the gingiva is attached to the tooth at the cemento-enamel junction. In disease, the position can be shifted either coronally (pseudopocket) or apical to the cemento-enamel junction (gingival recession).
Definition
Gingival recession is defined as the exposure of the root surface by an apical shift in the position of the gingiva.
Types
There are two types of recession i.e., visible, which is clinically observable and hidden, which is covered by gingiva and can only be measured with probe. Gingival recession may also be localized or generalized.
Position of the gingiva can be actual or apparent. Actual position is the level of epithelial attachment on the tooth i.e., from the cemento-enamel junction to the probable depth of the pocket, whereas apparent position is the level of crest of the gingival margin i.e., from the cemento-enamel junction to the gingival margin.
Classification of Gingival Recession
Two classification systems are available:
- According to Sullivan and Atkins Shallow-narrow, shallow-wide, deep-narrow and deep-wide.
- According to PD. Miller’s Class 1, Class II, Class III and Class IV.
Class I: Marginal tissue recession that does not extend to the mucogingival junction. There is no loss of bone or soft tissue in the interdental area. This can be narrow or wide.
Class II: Marginal tissue recession that extends to or beyond the mucogingival junction. There is no loss of bone or soft tissue in the interdental area. This can be narrow or wide.
Class III: Marginal tissue recession that extends to or beyond the mucogingival junction. In addition, there is loss of bone and/or soft tissue in the interdental area or there is malpositioning of the tooth.
Class IV: Marginal tissue recession that extends to or beyond the mucogingival junction with severe loss of bone and soft tissue interdentally and/or severe malpositioning of the tooth.
Prognosis of class I and II is good to excellent
Class III-only partial coverage can be expected
Class IV-Poor prognosis.
Etiology of Gingival Recession
Plaque-induced gingival inflammation is the primary etiological factor responsible for gingival recession; next most common cause is faulty tooth brushing. Other secondary/contributing factors of gingival recession are broadly categorized (for convenience) as:
- Anatomic factors
- Habits
- latrogenic factors
- Physilogic factors
- Anatomic factors include:
- Tooth malposition or position of the tooth in the arch. When a tooth is labially placed, the perio- dontium on the labial aspect will be invariably thin. When this is exposed to any kind of trauma or frictional forces, gingival recession results.
- Presence of dehiscence and fenestrations.
- Gingival ablation from soft tissues like cheek, lips,etc.
- Root-bone angle and mesiodistal curvature of the tooth surface. In rotated and facially-displaced teeth, bony plates are either thinned or shortened and recession results from repeated trauma to the thin periodontal tissues.
b)Habits: Faulty tooth brushing or brushing with hard bristles may lead to gingival recession. Recently it has been noted that there may be a positive relationship between smoking and recession. But the exact mechanism is not reported.
c)latrogenic factors: Primary trauma from occlusion has been reported to cause gingival recession. Ortho- dontic movement in a labial direction and improper restorations can lead to gingival recession.
d)Physiologic factors: Gingival recession was thought to be a physiologic process related to aging. However, this idea was discarded because there was no convincing evidence for a physiologic shift of the gingival attachment.
Clinical Significance of Gingival Recession
- The exposed root surface may be extremely sensitive
- Hyperemia of the pulp may result due to gingival recession
- Interproximal recession creates oral hygiene problems thereby resulting in plaque accumulation.
- Finally it is aesthetically unacceptable.
Changes in Gingival Contour
Normally, marginal gingiva is scalloped and knife edged, whereas interdental papilla in the anterior region is pyramidal and posteriorly tent-shaped. The factors that maintain normal contour are, shape of the teeth and its alignment in the arch, location and size of the proximal contact and dimensions of facial and lingual gingival embrasures. In diseased conditions, the marginal gingiva may become rounded or rolled whereas interdental papilla can become blunt and flat .