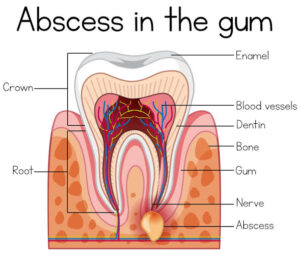
An abscess is a localized collection of pus, surrounded by an area of inflamed tissue in which hyperemia and infiltration of leukocytes is marked.
Radiographic Features:-

Bacteriology
Staphylococci are frequently associated with abscess formation. They produce the enzyme called coagulase which causes fibrin deposition and thus helps in walling off the lesion.
Coagulase promotes virulence by inhibiting phagocytosis.
• Small pockets of necrotic tissue are formed within cellulites, which coalesce and enlarge, compressing the surrounding fibrous connective tissue. Thus, an abscess is generated, which is a collection of pus surrounded by a wall of fibrous connective tissue.
Clinical Features :-

• Palpation when palpated clinically, a superficial abscess is fluctuant.
Offending tooth-offending tooth is carious and mobile.
Symptoms symptoms of acute inflammation, i.e. swelling and fever, are evident.
Acute Periapical Abscess :-
It is also called as acute alveolar abscess.
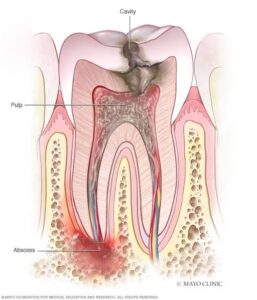
It is a localized collection of pus in the alveolar bone, at the root apex of a tooth, following death of the pulp.
Etiopathogenesis :-
It may be result of trauma or chemical mechanical irritation. The immediate cause is the or bacterial invasion of dead pulp.
The most common microorganism is Streptococcus viridans.
When inflammatory response may extend into adjacent periapical alveolar bone, it will initiate necrosis of periapical tissue and diffuse rarefaction of bone. leading to formation of periapical abscess with symptoms of acute inflammation.
Primary or necrotic abscess are pulpo-periapical inflammatory conditions associated with teeth, which have not developed apparent periapical radiolucent lesion; usually described as acute apical periodontitis or acute periapical abscess.
Canal contains large number of virulent bacteria that rapidly spread to periapically tissues, causing acute periodontitis, tender tooth and alveolar swelling.
Clinical features :-
Location-it develops in the periapical region of the tooth as sequelae to necrosis of pulp.
Symptoms :-
Pain is severe and of throbbing type.
Periapical abscess may confine to osseous structures and during the early period of abscess formation, may cause excruciating pain without observable swelling.
• The patient may appear pale, irritable and weak from pain, loss of sleep as well as from absorption of septic products.
He may have slight fever (99 to 100 F ).
Signs :-
Patients experience sensitivity or pressure in the affected area.
Ice relieves the pain and heat intensifies it aspiration yield yellowish pus.
• The tooth becomes more painful, appears elongated and mobile.
In acute periapical infection, tooth is sensitive to percussion and movement.
There is also painful lymphadenopathy.
After some period the affected pulp is necrotic and does not respond to electric current or to application of cold.
• Swelling is usually seen in adjacent tissues adjacent to the affected tooth..
Surface-the tissues at the surface of swelling appear taut and inflamed. The surface of tissue becomes distended from the pressure of underlying pus and finally ruptures due to pressure and lack of resistance caused by continued liquefaction.
Maxillary involvement-when the maxillary anterior teeth are involved, swelling of upper lip may extend to one or both eyelids. When the maxillary teeth
are involved, the cheek may swell to an immense size, distorting the patient’s face. When the maxillary posterior teeth are involved, there is possibility of maxillary sinus to involvement.
• Mandibular involvement-when the mandibular posterior teeth are involved, swelling of the cheek may extend to ear.
Radiographic features :-
Swelling of periodontal ligament space force the tooth slightly from its socket, creating widening of periodontal ligament space.
After some period, the first change is usually of slight unsharpness of some of the trabeculae at the tooth apex.
• If acute alveolar abscess of deciduous teeth occurs, the possibility of damage to the permanent successor can occur which is evident by rarefaction produced by destruction of the cortex of the follicle.
Histopathological features :-
• Central region of necrosis contains dense accumu- lation of polymorphonuclear leukocytes, sur- rounded by inflamed connective tissue wall of varying thickness.
Acute abscess contains necrotic and unidentical soft tissues.
There is an empty space, where suppuration has occurred.
The root canal appears to be devoid of tissue and instead, cups of microorganism and debris may be observed.
Bacteriology :-
Streptococci and staphylococci are generally recovered from the lesion.
Differential diagnosis :-
Periodontal abscess-it is an accumulation of pus along the root surface of a tooth. It is associated with periodontal pocket with mild pain. It is usually associated with vital, rather than pulp less teeth.
Management :-
Establish drainage immediately, if possible
May be done by opening the pulp chamber and passing file through the canal into the periapical region.
Trephination opening through mucosa and bore to the abscess at apex.
Through and through drain is placed in the abscess and irrigated with 1:1 mix of 3 percent
H₂O and normal saline solution.
Antibiotics like Penicillin 500 mg, qid, for 5 days and analgesics should be given.
In 24 to 48 hours, it can be determined if the tooth can be treated endodontically or extraction is necessary.
Warm saline mouth rinse often aid in localizing the infection and maintaining adequate drainage, before endodontic treatment or extraction.
If there is need of retention of offending tooth, necrotic pulp should be opened and tooth should be treated endodontically.