EXCHANGE OF RESPIRATORY GASES BETWEEN BLOOD AND ALVEOLI
The exchange of gases between blood and alveoli occurs only in the respiratory unit. It includes respiratory bronchio- les, alveolar ducts, atria, alveolar sacs and alveoli. The membrane through which the exchange occurs is called the respiratory membrane.
RESPIRATORY MEMBRANE
Respiratory membrane is formed by the epithelium of the respiratory unit and endothelium of pulmonary capillaries. The epithelium of the respiratory unit is a very thin membrane. As the capillaries are in close contact with this, the alveolar gases are in close proximity to the blood of the capillaries. This facilitates the gaseous exchange between air and blood .
Structure of Respiratory Membrane
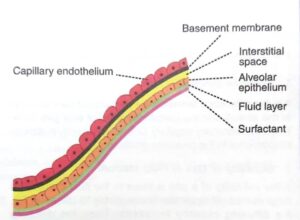
The respiratory membrane is formed by different layers of structures belonging to the alveoli and capillaries.
The gases diffuse through these layers. The different layers of respiratory membrane are as follows from within outside:
i. Monomolecular layer of surfactant, which spreads over the surface of the fluid lining of alveoli.
ii. A thin layer of fluid that lines the alveoli.
ii. The alveolar epithelial layer, which is composed of thin epithelial cells
iv. An interstitial space .
v. Basement membrane of capillary
vi. Capillary endothelial cells.
The average thickness of respiratory membrane is about 0.1 micron. The total surface area of the respiratory membrane in both the lungs is about 70 sq. meters.
The average diameter of pulmonary capillary is only 8 microns, which means that the red blood cells actually squeeze through the capillaries. Therefore, the membrane of red blood cells is having contact with capillary wall. This facilitates the quick exchange of oxygen and carbon dioxide between the blood and alveoli.
DIFFUSING CAPACITY
The exchange of gases occurs by bulk flow diffusion. The diffusion occurs due to pressure gradient. The diffusing capacity is defined as the volume of gas that diffuses through the respiratory membrane each minute for a pressure gradient of 1 mm Hg.
Diffusing Capacity for Oxygen and Carbon Dioxide :
Diffusing capacity for oxygen is 21 ml/minute/1 mm Hg. Diffusing capacity for carbon dioxide is 400 ml/minute/1 mmHg. Thus, the diffusing capacity for carbon dioxide is 20 times more than that of oxygen.
Factors Affecting Diffusing Capacity :
The diffusing capacity depends upon the following factors:
1. Pressure Gradient
It is the difference between the partial pressure of a gas in the alveoli and the partial pressure of that gas in the blood in pulmonary capillary. Diffusing capacity is directly proportional to the pressure gradient.
2. Solubility of Gas in Fluid Medium
If the solubility of a gas is more in the fluid medium, a large number of molecules are available for diffusion. So, the diffusing capacity increases. Thus, the diffusing capacity is directly proportional to solubility of the gas.
3. Total Surface Area of Respiratory Membrane
The surface area of respiratory membrane in each lung is about 70 sq m. If the total surface area of respiratory membrane is reduced, the diffusing capacity for the gases is reduced. So, the diffusing capacity is directly proportional to surface area of respiratory membrane. The diffusing capacity is reduced in emphysema since many of the alveoli are collapsed.
4. Molecular Weight of the Gas
If the molecular weight is more, the density is more and the rate of diffusion is less. So, the diffusing capacity is inversely proportional to molecular weight of the gas.
5. Thickness of Respiratory Membrane
More the thickness of respiratory membrane, less is the diffusion. Thus, the diffusion is inversely proportional to the thickness of the respiratory membrane. In conditions like fibrosis and edema, the diffusion rate is reduced because the thickness is increased.
■DIFFUSION OF OXYGEN
From Atmosphere to the Alveoli :
The partial pressure of oxygen in the atmosphere is 159 mm Hg and in the alveoli, it is 104 mm Hg. Because of the pressure gradient of 55 mm Hg, oxygen easily enters the alveoli from atmospheric air.
From Alveoli into the Blood :
The partial pressure of oxygen in the pulmonary capillary is 40 mm Hg and in the alveoli, it is 104 mm Hg. The pressure gradient is 64 mm Hg. This facilitates the diffu- sion of oxygen from alveoli into the blood .
Diffusion of oxygen from alveolus to pulmonary capillary

In the venous blood, the volume of oxygen is 14 ml%. The content of oxygen in arterial blood is 19 ml%. Thus,
Diffusion of carbon dioxide from pulmonary capillary to alveolus

the diffusion of oxygen from alveoli to blood is 5 ml/100 ml of blood.
DIFFUSION OF CARBON DIOXIDE
From Blood into Alveoli :
The partial pressure of carbon dioxide in alveoli is 40 mm Hg whereas in the blood it is 45 mm Hg. The pressure gradient of 5 mm Hg is responsible for the diffusion of carbon dioxide from blood into the alveoli (Fig. 124-3). The carbon dioxide content in the venous blood is 52 ml % and in arterial blood, it is 48 ml %. So, the diffusion of carbon dioxide from blood to alveoli is 4 ml/100 ml of blood.
From the Alveoli into the Atmosphere :
In the atmospheric air, the partial pressure of carbon dioxide is very insignificant and is only about 0.3 mm Hg whereas, in the alveoli, it is 40 mm Hg. So, carbon dioxide leaves alveoli easily.
EXCHANGE OF GASES BETWEEN BLOOD AND TISSUES
■DIFFUSION OF OXYGEN FROM BLOOD INTO THE TISSUES
Diffusion of oxygen from capillary to tissue
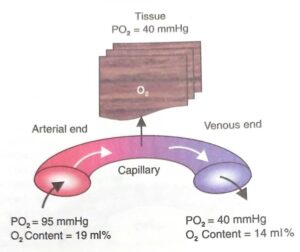
The partial pressure of oxygen in arterial blood is 95 mm Hg. This is because of admixture of venous blood resulted by 2% of shunt flow, i.e. 2% of blood reaches the heart without being oxygenated. The average oxygen tension in the tissues is only 40 mm Hg. This is because of continuous metabolic activity and oxygen is constantly utilized. Thus, a pressure gradient of about 55 mm Hg exists between blood and the tissues so that, oxygen can easily diffuse into the tissues .
The content of oxygen in arterial blood is 19 ml% and, in the venous blood, the volume of oxygen is 14 ml%. Thus, the diffusion of oxygen from blood to the tissues is 5 ml/100 ml of blood.
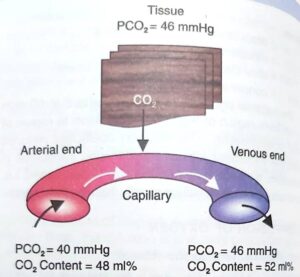
DIFFUSION OF CARBON DIOXIDE FROM TISSUES INTO THE BLOOD
Due to the continuous metabolic activity, carbon dioxide is produced constantly in the cells of the tissues. So, the partial pressure of carbon dioxide is high in the cells and is about 46 mm Hg. The partial pressure of carbon dioxide in arterial blood is 40 mm Hg. The pressure gradient of 6 mm Hg is responsible for the diffusion of carbon dioxide from tissues to the blood .
The carbon dioxide content in arterial blood is 48 ml%. And, in the venous blood, it is 52 ml%. So, the diffusion of carbon dioxide from tissues to the blood is 4 ml/100 ml of blood.
■RESPIRATORY EXCHANGE RATIO
Diffusion of carbon dioxide from tissues to capillary
The respiratory exchange ratio (R) is the ratio between the net output of carbon dioxide from the tissues to the simultaneous net uptake of oxygen by the tissues.
NORMAL VALUES
The value of R depends upon the metabolic activities. When a person utilizes only carbohydrates for body metabolism, R is 1.0. That means for during carbohydrate metabolism, the amount of carbon dioxide produced in the tissue is equal to the amount of oxygen consumed. If only fat is used for metabolism, the R is 0.7. When fat is utilized, oxygen reacts with fats and a large portion of oxygen combines with hydrogen ions to form water instead of carbon dioxide. Because of this, the carbon dioxide output is less than the oxygen consumed. So, the R is less. If only protein is utilized, R is 0.803.
However, when a balanced diet containing average quantity of proteins, carbohydrates and lipids is utilized, the R is about 0.825. In steady conditions, respiratory exchange ratio is equal to respiratory quotient.