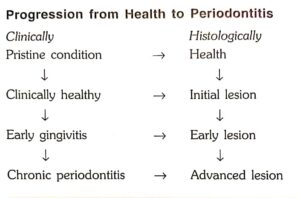
INTRODUCTION
Inflammation of gingiva is termed as gingivitis. The plaque microorganisms can exert its effect on perio- dontium by releasing certain products (e.g. collagenase, hyaluronidase, protease, chondroitin sulfatase) which can cause damage to the epithelial and connective tissue constituents. The intercellular spaces between the junctional epithelial cells are destroyed and may permit the bacterial products or bacteria themselves to gain access into the connective tissue .
The sequence of events during the development of gingivitis can occur in four different stages.
STAGE I GINGIVITIS: THE INITIAL VLESION
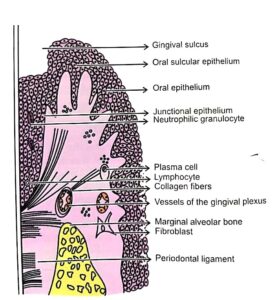
Normal marginal gingiva
Clinically, no visible changes are seen except presence of exudation of fluid from the gingival sulcus, hence this condition is called subclinical gingivitis.
The following features are observed in stage I gingivitis:
1. Classic vasculitis of vessels subjacent to the junctional epithelium.
2. Exudation of fluid from gingival sulcus.
3. Changes in the coronal most portion of the junctional epithelium.
Initial lesion
4. Increased migration of the leukocytes into the junctional epithelium and gingival sulcus.
5. Presence of serum, proteins.
6. Loss of perivascular collagen.
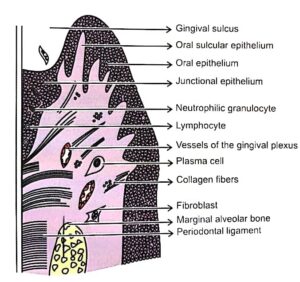
STAGE II GINGIVITIS: THE EARLY LESION
Early lesion
Clinically, erythematous gingiva and bleeding on probing may be evident. Microscopic features of the early lesion include:
1. All the changes seen in the initial lesion continue to intensify.
2. The junctional epithelium may begin to show the development of rete pegs or ridges.
3. Accumulation of lymphocytes (majority of them are T cells) beneath the junctional epithelium.
4. Further loss of collagen fibre network supporting the marginal gingiva.
5. Fibroblasts show cytotoxic alteration with a decreased capacity for collagen production.
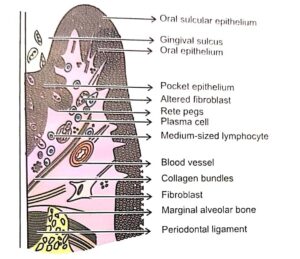
STAGE III GINGIVITIS: THE ESTABLISHED LESION
Clinical changes include:
a. A bluish hue on the reddened gingiva due to impaired venous return.
b. The gingiva appears to be moderately to severely inflammed.
Microscopically
1. Predominant inflammatory cell types are plasma cells, which invades epithelium and also deep into the connective tissue, around the blood vessels and between the bundles of collagen fibres.
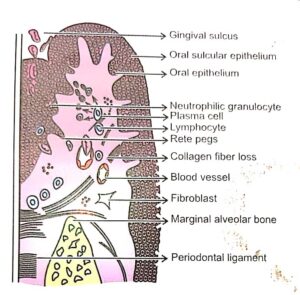 Established lesion.
Established lesion.- Proliferation, apical migration and lateral extension of the junctional epithelium is seen. Early pocket formation may or may not be presen
3. Further collagen destruction and continuing loss of connective tissue substance seen in the early lesion.
4. The following enzyme levels are said to be elevated in chronically inflammed gingiva, acid and alkaline phosphatase, B-glucuronidase, aminopeptidase and others.
STAGE IV GINGIVITIS: THE ADVANCED LESION
The advanced lesion is also known as phase of advanced periodontal breakdown.
The following clinical and microscopic features are seen:
1. Persistence of features described in the established lesion.
2. Extension of the lesion into the alveolar bone and periodontal ligament leading to significant amount of bone loss.
3. Continued loss of collagen.
4. Formation of periodontal pockets.
5. Conversion of bone marrow into fibrous tissue.
6. Presence of almost all the types of inflammatory cells.