GINGIVECTOMY

Gingivectomy means excision of the gingiva. By removing the pocket wall, gingivectomy provides visibility and accessibility for complete calculus removal and thorough smoothing of the roots, creating a favorable environment for gingival healing and restoration of a physiologic gingival contour.
The gingivectomy technique was widely performed in the past. Improved understanding of healing mechanisms and the development of more sophisticated flap methods have relegated the gingivectomy to a lesser role in the current repertoire of available techniques. However, it remains an effective form of treatment when indicated.
Indications and Contraindications
The gingivectomy technique may be performed for the following indications :
1. Elimination of suprabony pockets, regardless of their depth, if the pocket wall is fibrous and firm.
2. Elimination of gingival enlargements.
3. Elimination of suprabony periodontal abscesses.
Contraindications to gingivectomy include the following:
1. The need for bone surgery or examination of the bone shape and morphology.
2. Situations in which the bottom of the pocket is apical to the mucogingival junction.
3. Esthetic considerations, particularly in the anterior maxilla.
The gingivectomy technique may be performed by means of scalpels, electrodes, lasers, or chemicals. All these techniques are reviewed here, although the surgical method is the only technique recommended.
Surgical Gingivectomy

Step 1. The pockets on each surface are explored with a periodontal probe and marked with a pocket marker. Each pocket is marked in several areas to outline its course on each surface.
Step 2. Periodontal knives (e.g., Kirkland knives) are used for incisions on the facial and lingual surfaces and those distal to the terminal tooth in the arch. Orban periodontal knives are used for supplemental interdental incisions, if necessary, and Bard-Parker knives #11 and #12 and scissors are used as auxiliary instruments.
The incision is started apical to the points marking the course of the pockets 56 and is directed coronally to a point between the base of the pocket and the crest of the bone. It should be as close as possible to the bone without exposing it, to remove the soft tissue coronal to the bone. Exposure of bone is undesirable. If it occurs, healing usually presents no problem if the area is adequately covered by the periodontal pack.
Discontinuous or continuous incisions may be used . The incision should be beveled at approx- imately 45 degrees to the tooth surface and should recreate, as far as possible, the normal festooned pattern of the gingiva. Failure to bevel leaves a broad, fibrous plateau that takes more time than usually required to develop a physiologic contour. In the interim, plaque and food accumulation may lead to recurrence of pockets.
Step 3. Remove the excised pocket wall, clean the area, and closely examine the root surface. The most apical zone consists of a bandlike light zone where the tissues were attached, and coronally to it some calculus remnants, root caries, or root resorption may be found. Granulation tissue may be seen on the excised soft tissue .
Step 4. Carefully curette the granulation tissue, and remove any remaining calculus and necrotic cementum so as to leave a smooth and clean surface.
Step 5. Cover the area with a surgical pack .
Gingivoplasty :-

Gingivoplasty is similar to gingivectomy, but its purpose is different. Gingivectomy is performed to eliminate periodontal pockets and includes reshaping as part of the technique. Gingivoplasty is a reshaping of the gingiva to create physiologic gingival contours, with the sole purpose of recontouring the gingiva in the absence of pockets.
Gingival and periodontal disease often produce defor- mities in the gingiva that interfere with normal food excursion, collect plaque and food debris, and prolong and aggravate the disease process. Such deformities include
(1) gingival clefts and craters,
(2) shelflike inter- dental papillae caused by acute necrotizing ulcerative gingivitis, and
(3) gingival enlargements.
Gingivoplasty may be done with a periodontal knife, a scalpel, rotary coarse diamond stones,” or electrodes.13 It consists of procedures that resemble those performed in festooning artificial dentures: tapering the gingival margin, creating a scalloped marginal outline, thinning the attached gingiva, and creating vertical interdental grooves and shaping the interdental papillae to provide sluiceways for the passage of food.
Healing after Surgical Gingivectomy :-
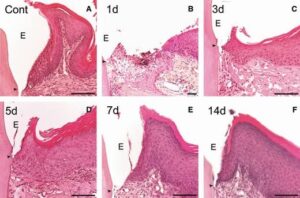
The initial response after gingivectomy is the formation of a protective surface clot; the underlying tissue becomes acutely inflamed, with some necrosis. The clot is then replaced by granulation tissue. By 24 hours, there is an increase in new connective tissue cells, mainly angio- blasts, just beneath the surface layer of inflammation and necrosis; by the third day, numerous young fibroblasts are located in the area.” The highly vascular granulation tissue grows coronally, creating a new, free gingival margin and sulcus.” Capillaries derived from blood vessels of the periodontal ligament migrate into the granulation tissue, and within 2 weeks, they connect with gingival vessels.
After 12 to 24 hours, epithelial cells at the margins of the wound start to migrate over the granulation tissue, separating it from the contaminated surface layer of the clot. Epithelial activity at the margins reaches a peak in 24 to 36 hours.The new epithelial cells arise from the basal and deeper spinous layers of the wound edge epithelium and migrate over the wound over a fibrin layer that is later resorbed and replaced by a connective tissue bed. The epithelial cells advance by a tumbling action, with the cells becoming fixed to the substrate by hemidesmosomes and a new basement lamina.
After 5 to 14 days, surface epithelialization is generally complete. During the first 4 weeks after gingivectomy, keratinization is less than it was before surgery. Complete epithelial repair takes about 1 month. Vasodilation and vascularity begin to decrease after the fourth day of healing and appear to be almost normal by the sixteenth day. Complete repair of the connective tissue takes about 7 weeks.
The flow of gingival fluid in humans is initially increased after gingivectomy and diminishes as healing progresses, Maximal flow is reached after 1 week, coinciding with the time of maximal inflammation.
Although the tissue changes that occur in post- gingivectomy healing are the same in all individuals, the time required for complete healing varies considerably, depending on the area of the cut surface and inter- ference from local irritation and infection. In patients with physiologic gingival melanosis, the pigmentation is diminished in the healed gingiva.
Gingivectomy by Electrosurgery :-

Advantages :
Electrosurgery permits an adequate contouring of the tissue and controls hemorrhage.
Disadvantages :
Electrosurgery cannot be used in patients who have noncompatible or poorly shielded cardiac pacemakers. The treatment causes an unpleasant odor. If the electrosurgery point touches the bone, irreparable damage can be done. Furthermore, the heat generated by injudicious use can cause tissue damage and loss of periodontal support when the electrode is used close to bone.
When the electrode touches the root, areas of cementum burn are produced. Therefore the use of electrosurgery should be limited to superficial procedures such as removal of gingival enlargements, gingivoplasty, relocation of frenum and muscle attachments, and incision of peri- odontal abscesses and pericoronal flaps; extreme care should be exercised to avoid contacting the tooth surface. Electro- surgery should not be used for procedures that involve proximity to the bone, such as flap operations, or for mucogingival surgery.
Technique :-
The removal of gingival enlargements and gingivoplasty is performed with the needle electrode, supplemented by the small, ovoid loop or the diamond-shaped electrodes for festooning. A blended cutting and coagulating (fully rectified) current is used. In all reshaping procedures, the electrode is activated and moved in a concise “shaving” motion.
In the treatment of acute periodontal abscesses, the incision to establish drainage can be made with the needle electrode without exerting painful pressure. The incision remains open because the edges are sealed by the current. After the acute symptoms subside, the regular procedure for the treatment of the periodontal abscess is followed .
For hemostasis, the ball electrode is used. Hemorrhage must be controlled by direct pressure (using air, compress, or hemostat) first; then the surface is lightly touched with a coagulating current. Electrosurgery is helpful for the control of isolated bleeding points. Bleeding areas located interproximally are reached with a thin, bar-shaped electrode.
Frenum and muscle attachments can be relocated to facilitate pocket elimination using a loop electrode. For this purpose, the frenum or muscle is stretched and sectioned with the loop electrode and a coagulating current. For cases of acute pericoronitis, drainage may be obtained by incising the flap with a bent-needle electrode. A loop electrode is used to remove the flap after the acute symptoms subside.
Healing after Electrosurgery :-
Some investigators report no significant differences in gingival healing after resection by electrosurgery and resection with periodontal knives. Other researchers find delayed healing, greater reduction in gingival height, and more bone injury after electrosurgery.” There appears to be little difference in the results obtained after shallow gingival resection with electrosurgery and that with periodontal knives. However, when used for deep resections close to bone, electrosurgery can produce gingival recession, bone necrosis and sequestration, loss of bone height, furcation exposure, and tooth mobility, which do not occur with the use of periodontal knives.
Laser Gingivectomy :-

The lasers most often used in dentistry are the carbon dioxide (CO2) and the neodymium:yttrium-aluminum- garnet (Nd:YAG), which have wavelengths of 10,600 nm and 1064 nm, respectively, both in the infrared range; they must be combined with other types of visible lasers for the beam to be seen and aimed.
The CO2, laser has been used for the excision of gingival growths, although healing is delayed compared with healing after conventional scalpel gingivectomy.” The use of a laser for oral surgery requires precautionary measures to avoid reflecting the beam on instrument surfaces, which could result in injury to neighboring tissues and the eyes of the operator.
Gingivectomy by Chemosurgery :-
Techniques to remove the gingiva using chemicals, such as 5% paraformaldehyde or potassium hydroxide, have been described in the past but are not currently used. They are presented here to provide a historical perspective.
The chemical gingivectomy has the following disadvantages:
The depth of action cannot be controlled, and therefore healthy attached tissue underlying the pocket may be injured.
Gingival remodeling cannot be accomplished effectively.
Epithelialization and re-formation of the junctional epithelium and reestablishment of the alveolar crest fiber system occur more slowly in chemically treated gingival wounds than in those produced by a scalpel.”
The use of chemical methods therefore is not recommended.