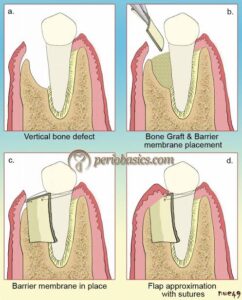
The method for the prevention of epithelial migration along the cemental wall of the pocket that has gained wide attention is guided tissue regeneration (GTR). This method derives from the classic studies of Nyman, Lindhe, Karring, and Gottlow and is based on the assumption that only the periodontal ligament cells have the potential for regenera- tion of the attachment apparatus of the tooth .
GTR consists of placing barriers of different types to cover the bone and periodontal ligament, thus temporarily separating them from the gingival epithelium. Excluding the epithelium and the gingival connective tissue from the root surface during the postsurgical healing phase not only prevents epithelial migration into the wound, but also favors repopulation of the area by cells from the periodontal ligament and the bone .
Initial animal experiments using Millipore filters and Teflon membranes resulted in regeneration of cementum and alveolar bone and a functional periodontal ligament. Clinical case reports showed GTR results in a gain in attachment level that is not necessarily asso- ciated with a buildup of alveolar bone.”, Histologic studies in humans provided evidence of periodontal reconstruction in most cases, even with horizontal bone loss.
The use of polytetrafluoroethylene (PTFE) membranes (Gore-Tex periodontal material, Gore-Tex, Flagstaff, Ariz) has been tested in controlled clinical studies in lower molar furcations and has shown statistically significant decreases in pocket depths and improvement in attach- ment levels after 6 months; bone level measurements have been inconclusive. A study on upper molar furcations did not result in significant gain in attachment or bone levels .
The initial membranes developed were nonresorbable and therefore required a second, although frequently simple, procedure to remove it. This second procedure done after the initial stages of healing, usually 3 to 6 weeks after the first intervention. The second procedure was a significant obstacle in the utilization of this GTR technique, and therefore resorbable membranes were developed.
The expanded polytetrafluoroethylene (ePTFE) membrane
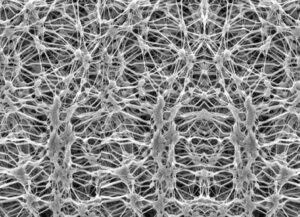
(nonresorbable) can be obtained in different shapes and sizes to suit proximal spaces and facial/lingual surfaces of furcations. The technique for its use is as follows:
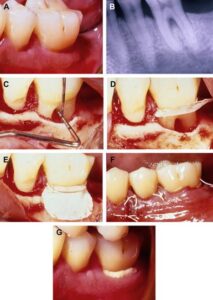
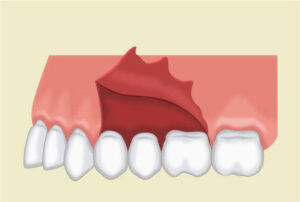
1. Raise a mucoperiosteal flap with vertical incisions, extending a minimum of two teeth anteriorly and one tooth distally to the tooth being treated.
2. Debride the osseous defect and thoroughly plane the roots.
3. Trim the membrane with sharp scissors to the approximate size of the area being treated. The apical border of the material should extend 3 to 4 mm apical to the margin of the defect and laterally 2 to 3 mm beyond the defect; the occlusal border of the membrane should be placed 2 mm apical to the cementoenamel junction.
4. Suture the membrane tightly around the tooth with a sling suture.

5. Suture the flap back in its original position or slightly coronal to it, using independent sutures interdentally and in the vertical incisions. The flap should cover the membrane completely.
6. The use of periodontal dressings is optional, and the patient receives antibiotic therapy for 1 week.
After 4 to 6 weeks, the margin of the membrane becomes exposed. The membrane is removed with a gentle tug 5 weeks after the procedure. If it cannot be removed easily, the tissues are anesthetized, and the material is surgically removed using a miniflap.
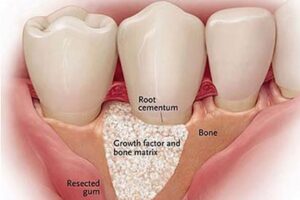
The results obtained with the GTR technique are enhanced when the technique is combined with grafts placed in the defects .
Combined Techniques :
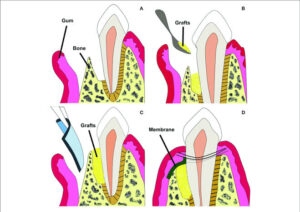
Several clinicians have proposed a combination of several of the techniques described in an attempt to enhance their results.
A classic paper published by Schallhorn and McClain in 1988 described a combination technique using graft material, root conditioning with citric acid, and coverage with a nonresorbable membrane (the only available one at the time). More recently, with the advent of osteopromotive agents, such as the enamel matrix derivative (Emdogain) and osteoconductive bovine- derived anorganic bone (Bio-Oss) graft materials, other combination techniques have been advocated. The combined use of these products, along with autogenous bone with resorbable membrane coverage, has resulted in an increased percentage of cases with successful new attachment and periodontal reconstruction .
Froum et al. have analyzed the criteria that should guide the choice of treatment technique. They believe that clinical results depend on
(1) The dimension and morphology of the defect (deeper lesions result in greater bone fill than shallower defects),
(2) The number of walls in the defect” (three-wall defects have greater potential to fill than two-wall or one-wall defects),
(3) The amount of root surface exposed and the ability to obtain adequate flap coverage,
(4) The angle of the defect to the long axis of the tooth (the smaller the angle, the better chance of success).