I. MECHANISM OF BREATHING
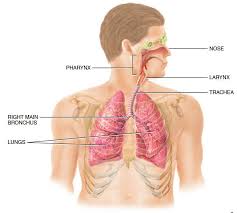
Eupnoea means rhythmic breathing at rest. It consists of Inspiration and Expiration.
Inspiration is an active process. During inspiration the size of the thoracic cavity is increased by contraction of appropriate muscles. The parietal pleura follows the expanding chest wall. The visceral pleura also follows the parietal pleura and thus the Elastic Lungs also follow the thoracic expansion passively. The expansion of lungs is associated with a fall in the pressure in the lung parenchyma and atmospheric air is thereby drawn into the depths of the lungs.
Expiration is a passive process. At the end of inspiration, the muscle which contracts actively during inspiration relaxes and the elastic recoil of the thoracic wall and lungs cause passive expiration.
At rest an adult breathes at a respiratory rate of 12-14 breaths/min and the amount of air inspired or expired per breath (i.e. Tidal Air) is approx. 500 ml. Thus, 6-7 litres of air is breathed in or out of the lungs per minute called Pulmonary Ventilation.
MECHANISM OF INSPIRATION
Inspiration is an ‘active’ process. During inspiration the thorax is enlarged by
A. movements of the ribs outwards and
upwards (Rib Movements); and
B. descent of the diaphragm (Diaphragmatic Movements)
A. Rib Movements
1. In quiet respiration, the first pair of ribs moves but little. In hypernoea their move- ments bring about increase in anteroposterior diameter of upper thorax.
2. The 2nd to 6th ribs slope obliquely downwards and forwards from their joints with the spinal column. On inspiration the ribs move upwards (Pump Handle Move- ments) to assume a more horizontal position due to contraction of external intercostal muscles (supplied by T12) to cause increase in anteroposterior diameter of the chest. Moreover, by virtue of their curved (bowed) mid-part, cause an increase in the transverse diameter of the thorax.
3. The lower ribs (7th to 10th) also swing
outwards and upwards (Bucket Handle
Movement) in inspiration to cause increase in the transverse diameter of the thorax.
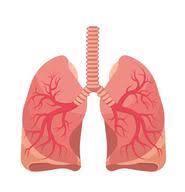
B. Diaphragmatic Movements
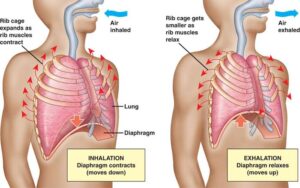
Diaphragm consists of muscle fibers which converge on the dome-shaped central tendinous portion.
During inspiration, as a result of discharge in phrenic neurons (C), muscle fibers contract and draw the central tendon downwards by 1.5 cm in eupnoea; and by 7 cm in deep inspiration. This causes an increase in the vertical diameter of the thoracic cage. For each 1 cm descent 200-300 ml of air is sucked in, therefore, diaphragmatic movements account for as much as 75% of tidal volume in eupnoea.
Accessory muscles of inspiration
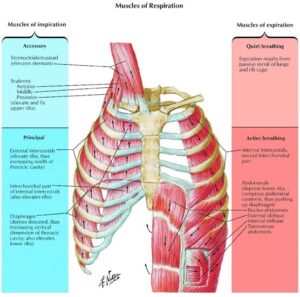
1. Scalene and sternocleidomastoid muscles in the neck play little, if any, part in breathing at rest, but become active in voluntary static inspiratory efforts and help to elevate the thoracic cage during deep inspiration.
2. Intrinsic muscles of the larynx: Abductor muscles of vocal cords i.e. posterior crico- arytenoid, contracts early in inspiratory phase pulling the vocal cords apart and opening the glottis. It is supplied by recurrent laryngeal nerve, a branch of vagus nerve.
MECHANISM OF EXPIRATION
In quiet breathing, expiration is a Passive Process, but during forced expiration, for example: voluntary expiratory efforts; during exercise; bronchial asthma etc.; the muscles of expiration contract, which include:
A. Anterior abdominal wall muscles (abdominal recti; transversus abdomi- nis; internal and external oblique muscles); and
B. Internal intercostal muscles.
1. Contraction of anterior abdominal wall muscles increases intra-abdominal pressure and draws the lower ribs down and medially, thereby pushing the diaphragm upwards, thus, aiding in expiration.
2. Internal intercostal muscles: They pass obliquely downwards and posteriorly from rib to rib. On contraction they pull the upper ribs down so that the ribs acquire the position as seen at the end of expiration.
3. Accessory muscles of expiration are adductor muscles of vocal cords. They begin to contract early in expiration, but their contraction is not complete. Therefore, it seems their main respiratory function is protective i.e. prevent entry of food and fluid into the trachea.
II. PRESSURE CHANGES DURING VENTILATION
(A) INTRA-PULMONARY (OR INTRA-
ALVEOLAR) PRESSURE
The expansion of lungs is attended by a fall in the pressure in the lungs parenchyma, called Intra Pulmonary Pressure or Intra Alveolar Pressure, so that air is pulled into the lungs via the tracheo-bronchial tree.
In quiet breathing, at end-expiration and at end-inspiration, as no air is going in and coming out of the lungs, therefore, intra- pulmonary pressure is equal to the atmos- pheric pressure (normal: 760 mmHg).
With the beginning of inspiration, as volume increases pressure decreases, therefore, the intra-pulmonary pressure decreases to approx. 3 mmHg below atmospheric pressure (i.e. 757 mmHg), but regains the full atmospheric pressure value at end-inspiration. When expiration follows passively, the elastic recoil of the lungs causes the intra-pulmonary pressure to swing slightly to the positive side (3 mmHg i.e. 763 mmHg) but regains the atmospheric pressure value at end-expiration.
FACTORS AFFECTING INTRA- PULMONARY PRESSURE
1. Valsalva Manoeuvre i.e. forced expiration against a closed glottis, may produce a positive intra-pulmonary pressure of ≥ 100 mmHg above the atmospheric value.
2. Muller’s Manoeuvre i.e. forced inspiration against a closed glottis, can reduce the intra- pulmonary pressure to ≤80 mmHg below the atmospheric value.
(B) INTRA-PLEURAL (OR INTRA- THORACIC) PRESSURE

The lungs and the chest wall are elastic structures. At end-expiratory position, the tendency of the lungs to recoil from the chest wall is just balanced by the tendency of the chest wall to recoil in the opposite direction. This causes a slight subatmospheric pressure to develop, say -2 mmHg between the two layers of pleura at the start of inspiration, called intra-pleural pressure or intra-thoracic pressure.
The negative intra-pleural pressure is directly proportional to the amount of thoracic expansion which occurs. Therefore, during quiet inspiration (i.e. at rest), the lungs are pulled into a more expanded position causing intra-pleural pressure to decrease to about -6 mmHg. At the end of inspiration, the lung recoil begins to pull the chest back to the expiratory position; and at end-expiratory position where the recoil pressure of the lungs and chest wall balance, intra-pleural pressure returns back to -2 mmHg.
FACTORS AFFECTING INTRA-PLEURAL PRESSURE
1. Deep inspiration decreases it as much as 30 mmHg subatmospheric i.e. 730 mmHg.
2. Valsalva manoeuvre or sudden forceful expiratory movements; for example, coughing, defecation etc., increase intra-pleural pressure by 60-70 mmHg i.e. it becomes 820-830 mmHg.
3. Effect of gravity – because of gravitational forces, intra-pleural pressure in standing position is more negative (-7 mmHg) at the apices of lungs compared to the bases (-2 mmHg) i.e. 5 mmHg greater at the bases of the lungs than at the apex.
This is why during first part of inspiration, more of the inspired gas goes to the apices than bases of the lungs.
III. LUNG VOLUMES AND CAPACITIES
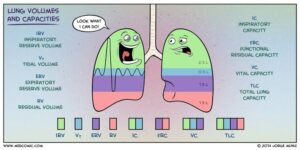
These can be divided into 2 major headings:
A. Static lung volumes and capacities (Time factor is not involved, therefore,
expressed in ml or L).
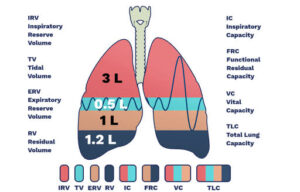
B. Dynamic lung volumes and capacities (Time dependent, therefore, expressed in ml/min or L/min).
A. STATIC LUNG VOLUMES AND
CAPACITIES
Volumes
1. Tidal Volume (TV). It is the volume of air breathed in or out of lungs, during quiet respiration. Normal: 500 ml.
2. Inspiratory Reserve Volume (IRV). It is the maximal volume of air which can be inspired after completing a normal tidal inspiration i.e. inspired from the end- inspiratory position. Normal: 2000-3200 ml. 3. Expiratory Reserve Volume (ERV). It is the maximal volume of air which can be expired after a normal tidal expiration i.e. expired from the end-expiratory position. Normal: 750-1000 ml.
4. Residual Volume (RV). It is the volume of air which remains in lungs after a maximal expiration. Normal: 1200 ml.
Capacities
1. Inspiratory Capacity (IC). It is the maximal volume of air which can be inspired after completing tidal expiration i.e. from the end-expiratory position. It can be computed as: TV + IRV. Normal: 2500-3700 ml.
2. Expiratory capacity (EC). It is the maximal volume of air which can be expired after completing tidal inspiration i.e. from the end-inspiratory position. It can be computed as: TV+ERV. Normal: 1250-1500 ml.
3.Vital Capacity (VC). It is the maximal volume of air which can be expelled from lungs, by forceful effort following a maximal inspiration.
Normal: 4.8 litres in males and 3.2 litres in females.
It can be computed as: TV + IRV + ERV.
ADVANTAGES OF VC
1. It provides useful information about the strength of the respiratory muscles; therefore, maximum inspiratory and expiratory effort can be assessed.
2. It gives the useful information about other aspects of pulmonary function through FEV,
FACTORS AFFECTING VC
A Physiological
(i) Physical dimension i.e. size and development of the subject. VC in males is 2.6 L/m² BSA; and in /females, 2.1 L/m² BSA. VC is more in males because of (a) large chest size, (b) more muscle power and (c) more BSA (body sur- face area).
(¡¡)Age: VC decreases in old age due to Toss of elasticity of lungs. (With aging, elastic fibers get replaced by fibrous tissue.)
(¡¡¡) Strength of respiratory muscles: VC increases in swimmers and divers.
(iv) Posture: in standing position VC is more as compared to sitting or lying positions, because in standing position,
(a) decrease in venous return, decreases the pulmonary blood flow and
(b) diaphragm descends down thus increasing inspiration.
(V) Pregnancy: VC decreases.
B. Pathological. VC decreases in diseases of the respiratory apparatus.
4. Functional Residual Capacity (FRC). It is the volume of air which is contained in the lungs at end-expiratory position i.e. after completion of tidal expiration. It can be computed as: RV + ERV. Normal: 2.5 litres.
‘FRC’ acts as a buffer and allows the continuous exchange of gases to occur even during expiration thereby prevents sudden changes in partial pressure of gases in the blood.
5. Total Lung Capacity (TLC). It is the volume of air contained in the lungs after a maximal inspiration. It can be computed as: VC+ RV. Normal: 6 litres.
B. DYNAMIC LUNG VOLUMES AND CAPACITIES
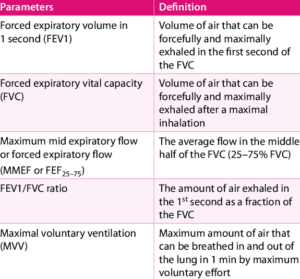
1. Timed Vital Capacity (TVC) or Forced
Vital Capacity (FVC)
If VC is recorded on a kymograph (spiro- graph) at the known speed, volume of air expelled can be timed. Thus, FVC is the maximum volume of air which can be breathed out as ‘forcefully’ and ‘rapidly’ as 216
possible following a maximum inspiration. Thus TVC is exactly similar to VC except that there is a special stress on “rapid, forcible and complete exhalation”.
IV. ALVEOLAR SURFACE TENSION
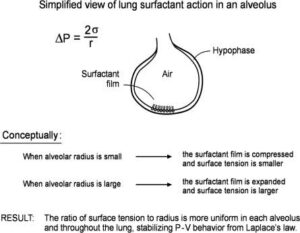
The lungs and the chest wall are elastic structures. The lungs are stretched when they are expanded at birth and at the end of resting expiration their tendency to recoil from the chest wall is just balanced by the tendency of the chest wall to recoil in the opposite direction. Thererfore, if the chest wall is opened the lungs collapse and if the lungs lose their elasticity, the chest expands and becomes barrel shaped.
The tendency of the lungs to recoil back from the chest wall is governed by two forces:
(1) Recoil of elastic tissue of the lungs, and
(2) Surface tension within the alveoli, due to the fact that alveoli contains a very thin film of fluid lining their inner side.
Surface tension is due to the intermolecular attraction between the surface molecules and thus it tries to reduce surface area and collapses the lungs. Hence this surface tension must be reduced especially during expiration. Otherwise, the lungs will collapse. Moreover, this force opposes the expansion of the lungs during inspiration.
V. PRESSURE VOLUME RELATIONSHIP: COMPLIANCE
A perfect elastic body like spring follows Hooke’s Law i.e. Length is directly propor- tional to Force (within the elastic limit). Therefore, greater the force applied, greater will be the length, but once the elastic limits are crossed, the spring tears off.
This relationship indicates stiffness and expansion of the spring. If line on the graph shifts towards left, it shows spring is more expandable i.e. less stiff. Conversely, if line on the graph shifts to right, it shows spring is less expandable i.e. more stiff.
Same law can be applied to the lungs and thorax which are elastic structures. In lungs we measure ‘volume’ equivalent to the length and ‘pressure’ equivalent to the force. Therefore, by increasing the airway pressure, lung volumes can be increased. However, in lungs, the above relationship will not be perfectly linear, as lungs and thorax are not perfect elastic structures. Here, this relationship indicates the distensibility (or stretchability) of lungs and thorax. This distensibility is called compliance. Therefore, compliance indicates the distensibility of the lungs and thorax.
VI. WORK DONE DURING BREATHING
To move the air into the lungs, the muscles of respiration have to do work to overcome all different forms of resistance. Therefore, work is done by the respiratory muscles:
(A) in stretching the elastic tissue of the
lungs and the chest wall, called Elastic Resistance. It is the force of elastic recoil exerted by the lung’s elastic fibers and force of surface tension;
(B) in moving viscous material of lung tissues, called Viscous Resistance;
(C) when air flows through the airways, there is resistance to the airflow, therefore, work is done in moving air through the respiratory passage, is called Airway Resistance.
Distribution of various forms of resistances, when expressed as percentage of the total resistance, is:
1. Elastic Resistance: 65%
2. Non-Elastic Resistance: 35%
(i) Viscous resistance: 7%
(ii) Airway resistance: 28%
VII. ALVEOLAR VENTILATION
(A) ALVEOLAR VENTILATION (V)
Alveolar ventilation is the amount of air
ventilating the alveoli per minute. Therefore, Alveolar Ventilation
= (Tidal Volume – Dead space ) × Respiratory Rate
(500-150) × 12
= 4.2 L/min.
Physiological significance of alveolar ventilation
Since respiration involves the gaseous
exchange of O, and CO, by diffusion between the alveoli and pulmonary capillary blood, therefore, maintenance of volume of alveolar ventilation is of paramount importance. All the factors which affect the tidal volume (TV), dead space (DS) and respiratory rate (RR), affect the alveolar ventilation. How?
In rapid shallow respiration (Tachypnoea), alveolar ventilation decreases though the pulmonary ventilation remains normal, as a result less air is available for exchange; while in slow and deep respiration, both alveolar and pulmonary ventilation are normal.
(B) DEAD SPACE
It is the amount of air in the ‘respiratory passage’ which does not take part in exchange of gases. It is of two types:
(1) Anatomical dead space (2) Physiological (total) dead space
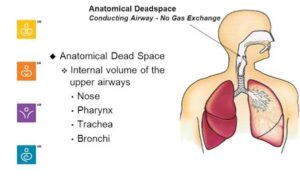
(1) Anatomical Dead Space
It is the volume of air present in the ‘conducting zone’ of the respiratory passage i.e. from nose and mouth upto terminal bronchioles where exchange of gases does not take place.
Normal value: 150 ml (approx. equal to the body weight in pounds).
(2) Physiological Dead Space or Total Dead Space
It includes anatomical dead space plus volume of air in the alveoli which does not take part in exchange of gases (ie. wasted alveolar ventilation).
For example,
(i) Volume of inspired air which ventilates alveoli but receives no pulmonary capillary blood flow; and
(ii) Some of the alveoli may be over ventilated i.e. volume of inspired air which ventilates alveoli in excess of that volume which is required to equilibrate with the blood.
Clinically anatomical and physiological dead spaces are same in healthy subjects. If ventilation and perfusion are not in equilibrium, then only they differ in volume.
Variations
1. Physiological
(i) Sex: DS is more in males.
(ii) Age: DS increases with age, because
inflated lungs pull the airways thereby
increasing the airway diameter.
(iii) Body height: DS increases in proportion with increase in body height.
2. Pathological: Diseases of the respiratory apparatus causes DS to increase.
(C) VENTILATION PERFUSION RATIO: VIP RATIO
It is the ratio of alveolar ventilation to
pulmonary blood flow.
As Alveolar ventilation is 4 L/min and Pulmonary blood flow, 5 L/min, therefore, ventilation perfusion ratio = 4 L/min divided by 5 L/min = 0.8.
Each lung normally displays the same ratio, receiving 2 L of air and 2.5 L of blood respectively.
But total ratio is not important. More important is that whether this ratio is present uniformly throughout the lungs for proper oxygenation. If it is not present, the oxygenation will be defective.
(D) DIFFUSION CAPACITY OF LUNGS
Definition: It is the amount of a gas that crosses the alveolar capillary membrane (respiratory membrane) per minute per mmHg difference in partial pressure of gas on the two sides of the membrane. Normal diffusion capacity for O2. (Do2)=
20-30 ml/min/mmHg at rest.
Factors affecting diffusion capacity (Dc)
1. Surface area and thickness of alveolar
capillary membrane.
Diffusion Capacity (Dc) =
Surface area of alveolar
capillary membrane (Normal: 70M2)
Thickness of alveolar capillary membrane (Normal: 0.5 µm)
In healthy subjects rapid diffusion of O2, and CO2, occurs within 0.3 secs across the alveolar capillary membrane. As Dc, varies directly with surface area and inversely with thickness of the alveolar capillary membrane, therefore,
(i) Dc of lungs decreases when there is block in pulmonary capillary or block in the airway because of decrease in surface area of the membrane.
(ii) Dc of lungs increases markedly (>3 times) in exercise because of increase in
surface area of the membrane due to
(a) opening of closed capillaries, and
(b) vasodilatation.
(iii) Dc of lungs decreases in pulmonary oedema due to collection of fluid in the alveolar capillary membrane which results in increased thickness of the membrane.