
Mucoepidermoid carcinoma is a malignant epithelial tumor, first studied and described as a separate entity by Stewart, Foote and Becker in 1945. As the name implies, the tumor is composed of both mucus-secreting cells and epidermoid-type cells in varying proportions. Columnar and clear cells are also seen, and often demonstrate prominent cystic growth. It is the most common malignant neoplasm observed in the major and minor salivary glands. Mucoepidermoid carcinoma represents 29-34 per cent of malignant tumors originating in both major and minor salivary glands. This carcinoma of the salivary glands accounts for 5 percent of all salivary gland tumors. The parotid gland is the most common site of occurrence. Intraorally, mucoepidermoid carcinoma shows a strong predilection for the palate.
Clinical Features.
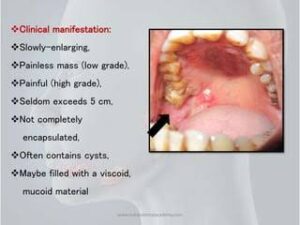
Mucoepidermoid carcinoma occurs with a slight female predilection. It occurs primarily in the third or fifth decades of life, with an average age of 47 years, but can occur in virtually all decades. It is the most common malignant salivary gland tumor of children. Prior exposure to ionizing radiation appears to substantially increase the risk of developing mucoepidermoid carcinoma.
The tumor of low-grade malignancy usually appears as a slowly enlarging, painless mass which simulates the pleomorphic adenoma. Unlike the pleomorphic adenoma, however, the low-grade mucoepidermoid carcinoma seldom exceeds 5 cm in diameter, is not completely encapsulated and often contains cysts which may be filled with a viscid, mucoid material. In addition to palate intrao- ral tumors occur on the buccal mucosa, tongue and retromolar areas. Because of their tendency to develop cystic areas, these intraoral lesions may bear close clinical resemblance to the mucous retention phenomenon or mucocele, especially those in the retromolar area .
The tumor of high-grade malignancy grows rapidly and does produce pain as an early symptom. Facial nerve paralysis is frequent in parotid tumors. The patient may also complain of trismus, drainage from the ear, dysphagia, numbness of the adjacent areas and ulceration, noted particularly in tumors of the minor salivary glands. The mucoepidermoid carcinoma is not encapsulated, but tends to infiltrate the surrounding tissue, and in a large percentage of cases, it metastasize to regional lymph nodes. Distant metastases to lung, bone, brain and subcutaneous tissues are also common.
Histologic Features.
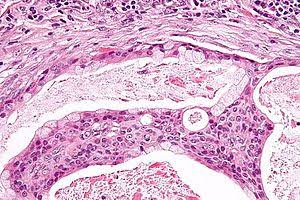
The mucoepidermoid carcinoma is composed of mucous secreting cells, epidermoid type (squamous) cells and intermediate cells. The mucous cells are of various shapes and have abundant, pale, foamy cytoplasm that stains positively for mucin stains. The epidermoid cells have squamodisc features, demonstrate a polygonal shape, intercellular bridges and rarely keratinization. A population of cells that is often more important in recognizing mucoepidermoid carcinoma is a group of highly prolific, basaloid cells referred to as the intermediate cells. These cells are larger than basal cells and smaller than the squamous cells and are believed to be the progenitor of epidermoid and mucous cells. Occasionally clusters of clear cells can be present. These clear cells are generally mucin and glycogen free. Epidermoid cells, together with intermediate and mucous cells line cystic spaces or form solid masses or cords. Epidermoid and mucous cells may be arranged in a glandular pattern. The cysts may rupture liberating mucus which may pool in the connective tissue and evoke an inflammatory reaction .
Mucoepidermoid carcinomas are graded as low-grade, intermediate-grade, and high-grade.
Low grade : tumors show well formed glandular structures and prominent mucin filled cystic spaces, minimal cellular atypia and a high proportion of mucous cells .
Intermediate grade : tumors have solid areas of epidermoid cells or squamous cells with intermediate basaloid cells. Cyst formation is seen but is less prominent than that observed in low grade tumors. All cell types are present, but intermediate cells predominate.
High grade : tumors consist of cells present as solid nests and cords of intermediate basaloid cells and epidermoid cells. Prominent nuclear pleomorphism and mitotic activity is noted. Cystic component is usually very less (<20 per cent). Glandular component is rare although occasionally it may predominate, Necrosis, and perineural invasion may be present.
Variants of Tumor :-
Sclerosing mucoepidermoid carcinoma :
Although mucoepidermoid carcinoma is the most common primary malignancy of the salivary glands, the sclerosing morphologic variant of this tumor is extremely rare, with only six reported cases. As its name suggests, sclerosing mucoepidermoid carcinoma is characterized by an intense central sclerosis that occupies the entirety of an otherwise typical tumor, frequently with an inflammatory infiltrate of plasma cells, eosinophils, and/or lymphocytes at its peripheral regions.
The sclerosis associated with these tumors may obscure their typical morphologic features and result in diagnostic difficulties. Tumor infarction and extravasation of mucin resulting in reactive fibrosis are two mechanisms that have been suggested as the cause of this morphologic variant.
Intraosseous mucoepidermoid carcinoma :

Mucoepidermoid carcinoma may originate within the jaws. This tumor type is known as central mucoepidermoid carcinoma. It is thought to form by the malignant transformation of the epithelial lining of odontogenic cysts. The tumor presents as an asymptomatic radiolucent lesion and is histologically of low grade malignancy. The mandible is three times more commonly affected than the maxilla.
Treatment and Prognosis :
Conservative excision with preservation of the facial nerve, if possible, is recommended for low and intermediate grade mucoepidermoid carcinomas of the parotid gland. The affected submandibular gland should be removed entirely. Radical neck dissection is performed in patients with clinical evidence of cervical node metastasis and is considered in any patient with a T3 lesion. Treatment for the minor glands is also primarily surgical. Some investigators have recommended postoperative irradiation only for high-grade malignancies, including high- grade mucoepidermoid carcinomas of the parotid glands. Few studies have assessed the role of chemotherapy and showed that high-grade mucoepidermoid carcinoma may show sensitivity similar to that of squamous cell carcinoma. Low- grade lesions had a five-year cure rate of 92 per cent, whereas the intermediate-grade and high- grade lesions had a 49 per cent five-year cure rate.