
It is a well established fact that the primary etiological agent in periodontal disease is bacterial plaque. The toxins and enzymes produced by the bacterial plaque elicit inflammatory and immunologic changes in the periodontal tissues at both cellular and molecular levels. These responses can be affected by a variety of systemic factors that can alter the response of the tissue to plaque. Further more, certain systemic disorders can have a direct effect on the periodontal tissues and these represent the periodontal manifestations of systemic diseases. In general these diseases do not initiate chronic destructive periodontitis but may accelerate its progression and increase tissue destruction.
DIETARY AND NUTRITIONAL ASPECTS OF PERIODONTAL DISEASE
The vitality of periodontal tissues, in both health and disease depends strongly on the essential nutrients. The epithelium of the dentogingival junction and the under- lying connective tissues are the most dynamic tissues.
The majority of opinions and research findings point to the following:
1. Nutritional deficiencies produce changes in the oral cavity.
2. There are no nutritional deficiencies that by them- selves cause gingivitis or periodontal pockets.
The Consistency of Diet :
From the viewpoint of promoting and maintaining gingival and periodontal health it is often stated that a firm and fibrous diet is more beneficial than an intake of soft and more loosely-textured food. Softer diets tend to produce greater deposits of plaque and an increase in plaque can be noticed, when the soft diet especially contains high proportion of sucrose. Diets that are predominantly fibrous are considered advantageous as they posses the ability to impart a natural cleansing action to the teeth and the periodontium.
A coarse diet, requires vigorous mastication and the plaque that forms approximately tends to be towards the cleansable buccal and lingual surfaces of the teeth. However coarse and granular diets can predispose to a direct traumatic injury to the supporting tissues.
Protein Deficiency and Periodontal Disease :

Proteins are constituents of the organic matrices of all the dental tissues including the alveolar bone. The integrity of the periodontal ligament is also dependent upon proteins (amino acid). Studies have indicated that on deprivation of proteins, extreme pathologic changes occur and there is marked degeneration of periodontal support.
Vitamins and Periodontal Disease :
Vitamins are essential, biologically-active constituents of a diet which cannot be replaced by other dietary components.
Vitamin C :
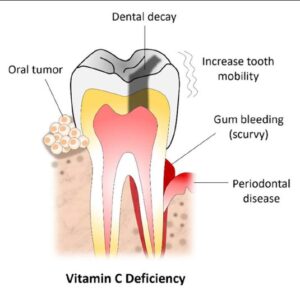
As deficiency in humans results in scurvy, a disease characterized by hemorrhagic diathesis and retardation of wound healing.
Clinical manifestations
1. Increased susceptibility to infections.
2. Impaired wound healing.
3. Bleeding and swollen gums.

4. Mobile teeth.

Histopathological features
1. Defective formation and maintenance of collagen.
2. Retardation or cessation of osteoid formation and impaired osteoblastic function.
3. Increased capillary permeability.
4. Susceptibility to traumatic hemorrhage.
5. Hyporeactivity of contractile elements of the peripheral blood vessels.
6. Sluggishness of blood flow.
Possible Etiologic Relationships between Ascorbic Acid and Periodontal Disease :
1. Low levels of Ascorbic acid influences the metabolism of collagen within the periodontium, thereby affecting the ability of the tissue to regenerate and repair by itself.
2. It interferes with bone formation leading to the loss of the alveolar bone.
3. Increases the permeability of oral mucosa to tritiated endotoxin and inulin.
4. Increased levels of Ascorbic acid enhances both the chemotactic and migratory action of leukocytes without influencing phagocytic activity.
5. Optimal level of Ascorbic acid is required to maintain the integrity of the periodontal microvasculature as well as the vascular response to bacterial irritation and wound healing.
6. Depletion of vitamin C may interfere with the ecologic equilibrium of bacteria in plaque and increases its pathogenicity.
Periodontal Features of Scurvy :
The oral symptoms are that of chronic gingivitis which can involve the free gingiva, attached gingiva and alveolar mucosa. In severe cases the gingiva becomes brilliant- red, tender and grossly swollen. The spongy tissues are extremely hyperemic and bleed spontaneously. In long standing cases the tissues attain a dark blue or purple hue. Alveolar bone resorption with increased tooth mobility has also been reported.
Vitamin D Deficiency :

Vitamin D is essential for the absorption of calcium from the gastrointestinal tract and the maintenance of calcium- phosphorus balance.
Radiographically, there is a generalized partial to complete disappearance of the lamina dura and reduced density of supporting bone, loss of trabeculae, increased radiolucency of the trabecular interstices and increased prominence of the remaining trabeculae.
Vitamin E :
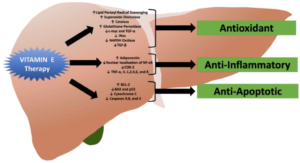
Evidence suggests that vitamin E acts as a antioxidant and plays an important role in maintaining the stability of cell membranes and protecting blood cells against hemolysis.
The possible role is based upon its ability to interfere with the production of prostaglandins.
Vitamin A :
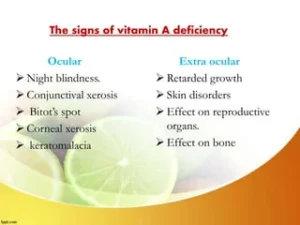
It is essential for normal functions of the retina, for growth, differentiation and maintenance of epithelial tissues and for bone growth and embryonic development.
Vitamin B-Complex :
Oral disease is rarely due to a deficiency in just one component of the B-complex group. Oral changes common to-Vitamin B-complex deficiencies are gingivitis, glossitis, glossodynia, angular cheilitis and inflammation of the entire oral mucosa.