It is usually culmination of a long period of chronic periodontitis.
Pathogenesis :-
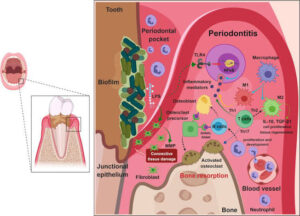
It usually occurs in pre-existing periodontal pocket. When such pocket reaches sufficient depth of about
5 to 8 mm, the soft tissues, around the neck of the tooth may approximate the tooth so tightly that orifice of the pocket is occluded.
Bacteria multiply in the depth of pocket and cause sufficient irritation to form an acute abscess, with exudation of pus into this area.

It results in sufficient swelling to destroy the cortical plates of bone.
Clinical features :-
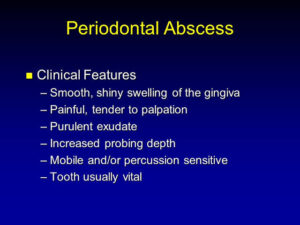
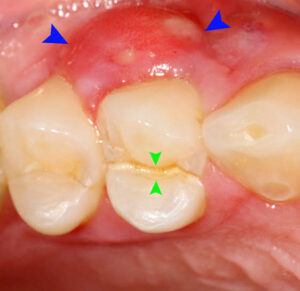
• Location it starts at the gingival cervice and extends down on one or more surface of the root, frequently as far as apical region.
Symptoms-acute episode usually has sudden onset with extreme pain. There is also distension and discomfort
• Signs :-

They are associated with swelling of the soft tissues overlying the surface of the involved root.
Tooth is tender on horizontal percussion and mobile.
Pus usually exudes from the gingival crevice.
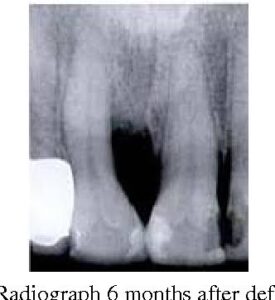
Radiographic features:-
Histopathological Features :
It consists of a central cavity filled with pus walled off on one side by the root and on the other side by connective tissue, as the epithelial lining of the crevice has been destroyed by the inflammatory process.
Management :-
• Primary treatment for relief of acute symptoms is incision of the fluctuant abscess, from the depth of the abscess cavity to the gingiva.
• The incision should extend into the soft tissues of the root surface.
• If the surrounding tissue is normal, the tooth may be retained and debridement of the root surface by removal of granulation tissue should be done. Treatment for new attachment and new tissue regeneration should be performed.
However, if the roots are denuded beyond the apical thirds of the root, the tooth should be extracted and curettage should be carried out to remove the granulation tissue from the socket.
ACUTE APICAL PERIODONTITIS :-

When the inflammatory degradation products from infected pulp penetrate, apically periodontal ligament in sufficient amount, inflammation is initiated .

Causes :-
Trauma-it may occur due to occlusal trauma caused by abnormal occlusal contact or by recently inserted restoration beyond the occlusal plane.
Wedging wedging of foreign object between the tooth such as toothpicks, food or a sliver of rubber dam left by teeth can cause inflammation.
Clinical Features :-
Location-inflammation is restricted to periodontal ligament.
Signs :-
.Tooth is non-sensitive to hot, cold, sweet or sour food.
Due to apical edema, tooth is elevated in the socket .
Very tender to pressure and percussion.
Symptoms-pain is of throbbing type.
Radiographic Features :-
• Widening of periodontal ligament space is caused by edema.
Histopathological Features :-
An inflammatory reaction occurs in the apical periodontal ligament.
• The blood vessels are dilated. Polymorphonuclear leukocytes are present and an accumulation of serous exudate distends the periodontal ligament and extrudes the tooth slightly.
Management :-
Determining the cause and relieving the symptoms.
• When the acute phase is subsided, the tooth is treated by conservative means.
ACUTE EXACERBATION OF A CHRONIC LESION :-
It is also called as phoenix abscess.
• It is an acute inflammatory reaction superimposed on an existing chronic lesion, such as on cyst or granuloma.
Causes :-
The periradicular area may react to noxious stimuli from a diseased pulp with chronic periradicular disease.
At times, because of an influx of necrotic product from a diseased pulp or because of bacteria and there toxins, this apparently dormant lesion may react and cause an acute inflammatory response.
Clinical Features :-
Signs at the onset, tooth may be tender to touch.
Symptoms patients complain of intense pain, local swelling and possibly associated cellulitis. .
Surface-mucosa over the radicular area may be sensitive to palpation and may appear red and swollen.
History-the patient has history of traumatic accident that turned the tooth dark after a period of time or of postoperative pain in a tooth that had subsided until the present episode of pain.
•Vitality test-lack of response to vitality test points to diagnosis necrotic pulp.
Histopathological Features :-
• Area of liquefaction necrosis with disintegrating polymorphonuclear neutrophils and cellular debris.
These are surrounded by infiltration of macrophages and some lymphocytes.
Differential Diagnosis :-
Acute alveolar abscess-vitality test; it will react to electrical pulp test and application of cold, as compared to acute exacerbation of chronic infection.
Management :-
• Drainage, either via the root canal or by incision, if there is localized swelling.