UNDISPLACED FLAP
Currently, the undisplaced flap may be the most frequently performed type of periodontal surgery. It differs from the modified Widman flap in that the soft tissue pocket wall is removed with the initial incision; thus it may be considered an “internal bevel gingivectomy.”
The undisplaced flap and the gingivectomy are the two techniques that surgically remove the pocket wall. To perform this technique without creating a mucogingival problem, the clinician should determine that enough attached gingiva will remain after removal of the pocket wall. The following steps outline the undisplaced flap technique:
Step 1: The pockets are measured with the periodontal probe, and a bleeding point is produced on the outer surface of the gingiva to mark the pocket bottom.
Step 2: The initial, or internal bevel, incision is made after the scalloping of the bleeding marks on the gingiva . The incision is usually carried to a point apical to the alveolar crest, depending on the thickness of the tissue. The thicker the tissue, the more apical is the ending point of the incision . In addition, thinning of the flap should be done with the initial incision because it is easier to accomplish at this time than later, with a loose, reflected flap that is difficult to manage.
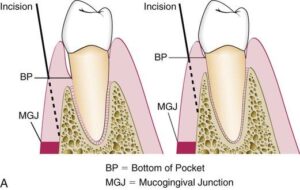
Internal bevel incision in Undisplaced Flap
Step 3: The second, or crevicular, incision is made from the bottom of the pocket to the bone to detach the connective tissue from the bone.
Step 4: The flap is reflected with a periosteal elevator (blunt dissection) from the internal bevel incision. Usually there is no need for vertical incisions because the flap is not displaced apically.
Step 5: The third, or interdental, incision is made with an interdental knife, separating the connective tissue from the bone.
Step 6: The triangular wedge of tissue created by the three incisions is removed with a curette.
Step 7: The area is debrided, removing all tissue tags and granulation tissue using sharp curettes.
Step 8: After the necessary scaling and root planing, the flap edge should rest on the root-bone junction. If this is not the case, because of improper location of the initial incision or the unexpected need for osseous surgery, the edge of the flap is rescalloped and trimmed to allow the flap edge to end at the root-bone junction.
Step 9: A continuous sling suture is used to secure the facial and the lingual or palatal flaps. This type of suture, using the tooth as an anchor, is advantageous to position and hold the flap edges at the root-bone junction. The area is covered with a periodontal pack.
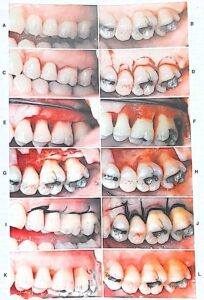
Undisplaced flap. A and B, Preoperative facial and palatal views.
C and D, Internal bevel incisions in the facial and palatal aspects.
Note the deeper scalloping palatally for the replaced flap. E and F, Flap elevated showing osseous defects.
G and H, Osseous surgery has been performed.
I and J, Flaps have been placed in their original site and sutured.
K and L, Postoperative results.